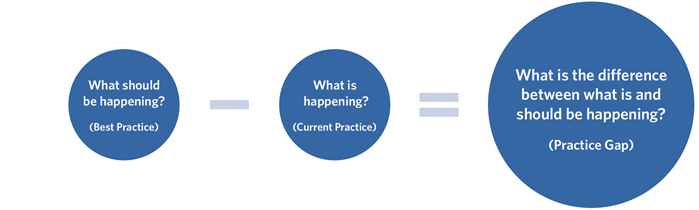
The space between the best practice (the answer to the question "What should be happening?") and the current practice (the answer to the question "What is currently happening?") reveals the gap (the answer to the question "What is the difference between what is and should be happening?").
Another way to approach a gap analysis is by answering the following questions:
What areas in practice do you and your colleagues find challenging?
Examples:
- Difficult-to-manage or non-resolvable cases
- Improving leadership ability
- Prevalent public health problems
- Patient safety concerns
- Limitations occurring in the healthcare system
What factors are contributing to an identified problem in practice?
Examples:
- Insufficient funding
- Lack of training
- Institutional bias/culture
What does the learner need to do differently in order to improve practice or professional skills?
Examples:
- Refine technical/procedural skills
- Learn and practice optimal communication strategies and techniques
- Collaborate interprofessionally for best patient outcomes
Guidelines to Identify Professional Practice/Patient Care Gaps
Below are common methods used to determine best practices and resulting practice gaps:
- Research findings/evidence
- Patient care audits/quality improvement data
- Current literature
- National clinical guidelines
- Trends in healthcare
- Expert feedback (planning committee or other committee of subject matter experts)
- Faculty feedback
- Consensus of experts and related committees
- Participant feedback
- Needs assessment results
- Previous CME activities evaluations or outcomes
- Regulatory body requirements
- State licensure requirements
- Board requirements
Gap Statement: CME Credit Application
The first three questions on the ACS CME Application section "Educational Activity Details" pertain to practice gaps and underlying educational needs that must be addressed when planning and developing a CME activity:
- What are the practice or patient care problems being addressed by this activity?
Example: Evidence has shown that an endoscopic approach has higher surgical risks compared with endoscopic approaches.
- Why do these issues exist? Is there a deficit in provider's knowledge or skill? Is there a deficit in health care system process or outcomes?
Example: Providers do not have sufficient knowledge of lowered complication rates in CTS release surgery.
- What methods have been used to determine the professional practice gap?
Example: Previous CME Activity, Evaluation, or Outcomes
Linking to Learning Objectives
When identifying practice gaps and the underlying educational needs, consider how an educational activity that addresses both should be designed. The resulting educational intervention must relate to increasing learner knowledge, competence, and/or performance (ACCME "Designed to Change" Requirement).
With at least one of these areas in mind, develop corresponding learning objectives.
Learning objectives clearly state what the learner will be able to do upon completion of a CME activity. Keeping the intended outcomes in mind when developing an educational activity helps to guide its structure and design, including the selection of educational formats and content that promote the achievement of these goals. Answering the question "What is the best format for teaching and learning the concepts to be presented?" may help in selecting the most effective educational format. Examples include:
- Didactic presentation (lecture)
- Demonstration of equipment/techniques
- Hands-on (skill-building) workshop
- Online modules
- Flipped classroom
- Team training
- Panel discussion
- Case-based work
- Simulation
- Self-directed
- Question and answer or quiz-based
- Use of standardized patients
The ACS CME Application contains questions related to each of these areas in order to prompt thoughtful consideration during the planning of the educational activity. In addition, learning objectives inform which evaluation and assessment tools should be utilized after an educational intervention, which help measure to which extent the intended goals were met. Refer to more information regarding writing effective learning objectives.
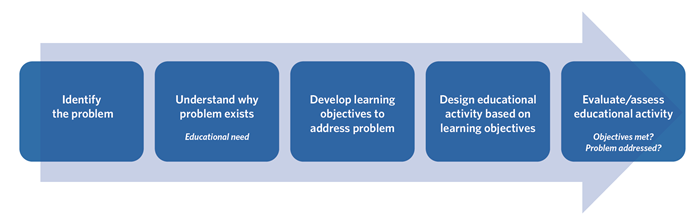
Practice Gaps: Key Points
- Identify the problem in practice ("practice gap")
- Consider the reason it exists (underlying educational need)
- Develop learning objectives for an educational intervention to close those gaps
- Design the educational activity around these objectives
- Evaluate whether the learning objectives were met
Additional Resources
Closing Practice Gaps: Educational Needs
References
ACCME. Addressing Practice Gaps. July 5, 2016. Available at: https://www.accme.org/resources/video-resources/accreditation-requirements/addressing-practice-gaps. Accessed May 2020. Wittich CM, Chutka DS, Mauck KF, Berger RA, Litin SC, Beckman TJ. Perspective:
A practical approach to defining professional practice gaps for continuing medical education. Acad Med. 2012;87(5):582‐585. doi:10.1097/ACM.0b013e31824d4d5f