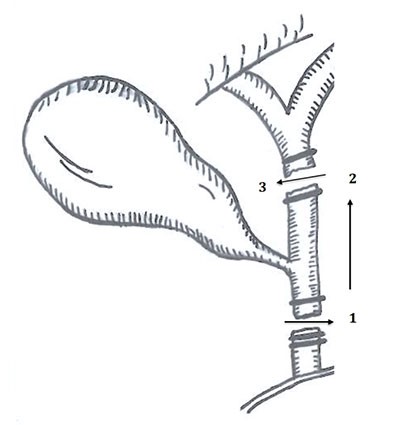
Figure 4. Hepp-Couinaud Roux-en-Y hepaticojejunostomy reconstruction.
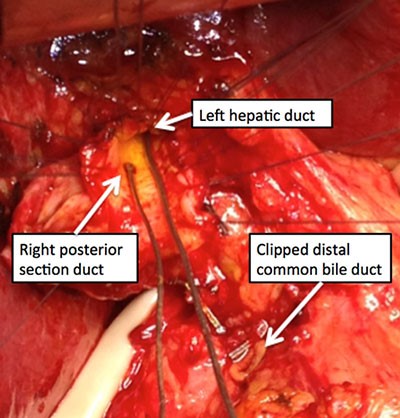
After removing the gallbladder and clearing all stones, we performed a Hepp-Couinaud Roux-en-Y hepaticojejunostomy to the common bile duct at the level of the right posterior duct insertion. The lumen measured approximately 2.5cm. The transected distal common bile duct was clipped by the transferring surgeon and we left this alone. Two drains were placed to monitor for bile leak post operatively. The final pathology demonstrated chronic cholecystitis with wall thickening and congestion in addition to cholelithiasis.
The patient recovered well with no evidence of bile leak and his drains were discontinued prior to discharge home on postoperative day five. At his four-week follow-up visit, he had returned to normal activities, tolerated a normal diet, and had only a mildly elevated alkaline phosphatase with normal liver function tests otherwise. He has had no evidence of biliary obstruction, stricture, or complications at 5.2-year follow-up. It is important to note that the patient was very satisfied with his care by his original surgeon. He even chose to have his follow-up with the first surgeon in order to avoid travel and time away from home.
Discussion
Bile duct injuries continue to occur in laparoscopic cholecystectomy even after more than two decades have passed since the procedure was introduced. A number of proposed methods of safety have been employed with various approaches to confirming and/or documenting biliary anatomy.2-6 The critical view of safety approach is indeed protective but has variable understanding and use by practicing surgeons.7-10 In addition, evidence supports that the critical view of safety approach is not the only safe method and that attempting to complete a critical view of safety can lead to biliary injury in densely inflamed tissue or in the case of aberrant anatomy.11,12 We also know that converting to an open cholecystectomy may lead to more complex injury in unskilled hands or those less familiar with complicated laparoscopic cholecystectomy.13 Proposed surgeon competencies and algorithms for safe cholecystectomy have attempted to create a framework to avoid bile duct injuries.14,15 Despite these efforts, it is still common for hepatobiliary surgeons to accept high-level bile duct injuries, for operative management and reconstruction.
To our knowledge, a case of bile duct injury in which the surgeon stopped resective surgery and the gallbladder was left in situ has not been reported in the literature. Because this phenomenon cannot be easily studied, we demonstrate that the patient in this case was likely spared significant morbidity because the transferring surgeon wisely stopped and reassessed the situation when injury was suspected rather than completing the cholecystectomy. From our experience, this is usually not the case and patients with biliary injury most often arrive without their gallbladder and higher levels of injury, thus requiring more complex operative repair. A review of biliary injury in 112 patients found that 71.6% of biliary injuries were E2–E5 and not one patient with an E1 injury had long-term complications.16 Personal communication with Strasberg, the primary author, reported that not one of the biliary injuries referred to their facility arrived with a gallbladder in situ. This is likely why high-level injuries occur.
E1 injuries have the best long-term outcomes, least risk of stricture, and least risk of concomitant vasculobiliary injury. It is indeed our current advice and teaching to all surgeons that perform laparoscopic cholecystectomy that when a bile duct injury is suspected, a pause should be initiated. Importantly, if an injury is identified and a qualified colleague is available, immediate intraoperative consultation should be initiated to assist with collaborative decision-making and reconstruction, if appropriate. What happens after that pause depends on the surgeon’s ability and resources, as well as adhering to the foundation of medicine to do no harm or, in some cases, do no further harm.
Conclusion
This case suggests that avoiding further resective surgery likely results in less severe biliary injury, better long-term outcomes, and more satisfied patients. It is time to change the culture of safe cholecystectomy to include stopping surgery when one suspects a bile duct injury and, thus, avoiding a secondary injury to the biliary system.17,18
Lessons Learned
Biliary injury is a highly morbid event in laparoscopic cholecystectomy. Leaving the gallbladder in situ and abandoning the perceived need to complete the laparoscopic cholecystectomy may prevent higher grades of biliary injury and reduce harm to patients.
Authors
Deal SBa, Alseidi AAb
Correspondence Author
Shanley B. Deal, MD
Virginia Mason Medical Center
Graduate Medical Education
Mailstop H8-GME
1100 9th Avenue
Seattle, WA 98101
253-948-6920
Shanley.Deal@virginiamason.org
Author Affiliations
- Virginia Mason Medical Center, Graduate Medical Education, Mailstop H8-GME, 1100 9th Ave., Seattle, WA 98101
- Virginia Mason Medical Center, Department of General, Thoracic, and Vascular Surgery, Mailstop C6-GS, 1100 9th Ave., Seattle, WA 98101
References
- Strasberg SM, Helton WS. An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB (Oxford). 2011;13(1):1-14.
- Buddingh KT, Hofker HS, ten Cate Hoedemaker HO, van Dam GM, Ploeg RJ, Nieuwenhuijs VB. Safety measures during cholecystectomy: results of a nationwide survey. World J Surg. 2011;35(6):1235-41; discussion 42-3.
- Buddingh KT, Morks AN, ten Cate Hoedemaker HO, Blaauw CB, van Dam GM, Ploeg RJ, et al. Documenting correct assessment of biliary anatomy during laparoscopic cholecystectomy. Surg Endosc. 2012;26(1):79-85.
- Buddingh KT, Nieuwenhuijs VB. The critical view of safety and routine intraoperative cholangiography complement each other as safety measures during cholecystectomy. J Gastrointest Surg. 2011;15(6):1069-70; author reply 71.
- Buddingh KT, Nieuwenhuijs VB, van Buuren L, Hulscher JB, de Jong JS, van Dam GM. Intraoperative assessment of biliary anatomy for prevention of bile duct injury: a review of current and future patient safety interventions. Surg Endosc. 2011;25(8):2449-61.
- Buddingh KT, Weersma RK, Savenije RA, van Dam GM, Nieuwenhuijs VB. Lower rate of major bile duct injury and increased intraoperative management of common bile duct stones after implementation of routine intraoperative cholangiography. J Am Coll Surg. 2011;213(2):267-74.
- Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the "critical view of safety" technique. J Gastrointest Surg. 2009;13(3):498-503.
- Daly SC, Deziel DJ, Li X, Thaqi M, Millikan KW, Myers JA, et al. Current practices in biliary surgery: Do we practice what we teach? Surg Endosc. 2016;30(8):3345-50.
- Stefanidis D, Chintalapudi N, Anderson-Montoya B, Oommen B, Tobben D, Pimentel M. How often do surgeons obtain the critical view of safety during laparoscopic cholecystectomy? Surg Endosc. 2017;31(1):142-6.
- Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 2010;211(1):132-8.
- Hibi T, Iwashita Y, Ohyama T, Honda G, Yoshida M, Takada T, et al. The "right" way is not always popular: comparison of surgeons' perceptions during laparoscopic cholecystectomy for acute cholecystitis among experts from Japan, Korea and Taiwan. J Hepatobiliary Pancreat Sci. 2017;24(1):24-32.
- Strasberg SM, Brunt LM. The Critical View of Safety: Why It Is Not the Only Method of Ductal Identification Within the Standard of Care in Laparoscopic Cholecystectomy. Ann Surg. 2017;265(3):464-5.
- Booij KA, de Reuver PR, Nijsse B, Busch OR, van Gulik TM, Gouma DJ. Insufficient safety measures reported in operation notes of complicated laparoscopic cholecystectomies. Surgery. 2014;155(3):384-9.
- Madani A, Watanabe Y, Feldman LS, Vassiliou MC, Barkun JS, Fried GM, et al. Expert Intraoperative Judgment and Decision-Making: Defining the Cognitive Competencies for Safe Laparoscopic Cholecystectomy. J Am Coll Surg. 2015;221(5):931-40 e8.
- Hori T, Oike F, Furuyama H, Machimoto T, Kadokawa Y, Hata T, et al. Protocol for laparoscopic cholecystectomy: Is it rocket science? World J Gastroenterol. 2016;22(47):10287-303.
- Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM. "Sideways": results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg. 2009;249(3):426-34.
- Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc. 2015;29(11):3074-85.
- Strasberg SM. Biliary injury in laparoscopic surgery: part 2. Changing the culture of cholecystectomy. J Am Coll Surg. 2005;201(4):604-11.