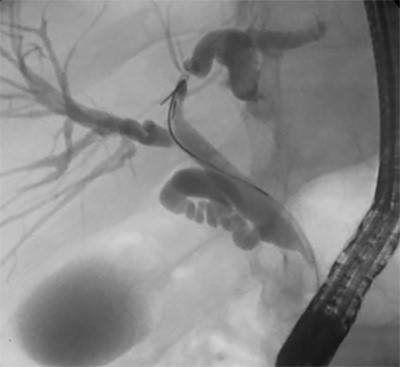
Figure 6. The specimen demonstrating chronic, pigmented, intrahepatic stones and a diseased left bile duct with associated stricture.
Discussion
RPC due to pyogenic bile duct infection has an associated high morbidity and mortality.8,9 As such, it is a challenging surgical disease to manage and evidence supports hepatectomy for definitive management.9 This case report reviews methods and techniques that the surgeon should use during parenchymal transection in order to avoid intrahepatic misadventure and straying from the planned transection path.
This case highlights a step-wise approach to laparoscopic liver resection using cognitive task analysis to break down the operation into discrete tasks (Table 1). Details for each step are summarized to help educate surgeons planning to incorporate this advanced skill in their practice or to improve their current approach to laparoscopic liver surgery. This approach is also provided at 10
|
Operative Step
|
Action
|
|
1. Liver mobilization
|
Mobilize the suprahepatic vena cava, left coronary ligament, and left triangular ligament
Start: Falciform ligament
End: Triangular ligament
|
|
2. Take down gallbladder adhesions
|
Dense adhesions from recurrent episodes of inflammation need to be taken down.
Start: Gallbladder anterior fundus
End: Adhesions clear enough to mobilize liver well
|
|
3. Isolate the hepatoduodenal (HDL) ligament
|
Clear the lesser sac and right lateral aspect of the portal pedicle
Start: Recreate the foramen of Winslow
End: Place Rumel tourniquet for Pringle maneuver
|
|
4. HDL dissection
|
Dissect the left hepatic artery and transect it, then dissect the left portal vein and transect it.
Start: Identify bifurcation to the left and right hepatic artery
End: Transect the left portal vein
|
|
5. Preparing for hepatic transection
|
Delineate a line of dissection to the left of the MHV using US and create a transection crevasse
Start: US suprahepatic liver
End: Transect 1.5cm deep crevasse along entire planned transection line
|
|
6. Hepatic transection using caudal approach
|
Parenchymal dissection along the US mapped & previously delineated crevasse
Start: Parenchymal dissection w/CUSA along delineation
End: Stop when left liver is suspended by the left bile duct
|
|
7. Bile duct exploration and complete the parenchymal dissection
|
Parenchymal dissection until left liver removed
Start: Transect bile duct and continue dissecting parenchyma along delineated plane supra-hepatically
End: Stapling of the left hepatic v.
|
|
8. Remove the gallbladder and hemostasis
|
Perform intraoperative cholangiogram (IOC) and remove the gallbladder
Start: Dissect hepatocystic triangle to achieve the critical view of safety
End: Remove gallbladder, retrieve specimen, confirm hemostasis and close trocar sites
|
Table 1. Operative steps for laparoscopic left liver resection using the caudal approach including specific actions, start and end, tips for success, and pitfalls/cautions for each step.
Conclusion
Definitive management of RPC via a laparoscopic hepatectomy with common bile duct exploration is a safe and effective approach. Cognitive task analysis can be used to break down a complex operation into modular tasks to educate surgeons how to incorporate each task in their practice or to improve their current approach to laparoscopic liver surgery.
Lessons Learned
Using cognitive task analysis, a complex laparoscopic liver resection can be divided into manageable tasks to educate surgeons adopting this operative technique. The principles highlighted in this case can be applied to laparoscopic liver surgery in many contexts and emphasize critical pitfalls and tips to promote a safe operation.
Authors
Deal SBa, Alseidi AAb
Correspondence Author
Shanley B. Deal, MD
Virginia Mason Medical Center
Graduate Medical Education
Mailstop H8-GME
1100 9th Avenue
Seattle, WA 98101
253-948-6920
Shanley.Deal@virginiamason.org
Author Affiliations
- Virginia Mason Medical Center
Graduate Medical Education
Mailstop H8-GME
1100 9th Avenue
Seattle, WA 98101
- Virginia Mason Medical Center
Department of General, Thoracic, and Vascular Surgery
Mailstop C6-GS
1100 9th Avenue
Seattle, WA 98101
Meeting Presentation
Seattle Surgical Society Annual Meeting, Seattle, WA, January 2017
Disclosures
Drs. Deal and Alseidi have no conflicts of interest or financial disclosures to report.
Acknowledgements
This research was supported by the Patterson Surgery Research Endowment.
References
- Clark RE, Pugh CM, Yates KA, Inaba K, Green DJ, Sullivan ME. The use of cognitive task analysis to improve instructional descriptions of procedures. J Surg Res. 2012;173(1):e37-42.
- Sullivan ME, Brown CV, Peyre SE, Salim A, Martin M, Towfigh S, et al. The use of cognitive task analysis to improve the learning of percutaneous tracheostomy placement. Am J Surg. 2007;193(1):96-9.
- Sullivan ME, Ortega A, Wasserberg N, Kaufman H, Nyquist J, Clark R. Assessing the teaching of procedural skills: can cognitive task analysis add to our traditional teaching methods? Am J Surg. 2008;195(1):20-3.
- Sullivan ME, Yates KA, Inaba K, Lam L, Clark RE. The use of cognitive task analysis to reveal the instructional limitations of experts in the teaching of procedural skills. Acad Med. 2014;89(5):811-6.
- Soubrane O, Schwarz L, Cauchy F, Perotto LO, Brustia R, Bernard D, et al. A Conceptual Technique for Laparoscopic Right Hepatectomy Based on Facts and Oncologic Principles: The Caudal Approach. Ann Surg. 2015;261(6):1226-31.
- Tomishige H, Morise Z, Kawabe N, Nagata H, Ohshima H, Kawase J, et al. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J Gastrointest Surg. 2013;5(6):173-7.
- Morise Z. Laparoscopic liver resection for posterosuperior tumors using caudal approach and postural changes: A new technical approach. World J Gastroenterol. 2016;22(47):10267-74.
- Verweij KE, van Buuren H. Oriental cholangiohepatitis (recurrent pyogenic cholangitis): a case series from the Netherlands and brief review of the literature. Neth J Med. 2016;74(9):401-5.
- Tabrizian P, Jibara G, Shrager B, Schwartz ME, Roayaie S. Hepatic resection for primary hepatolithiasis: a single-center Western experience. J Am Coll Surg. 2012;215(5):622-6.
- Deal SB, Alseidi A. Laparoscopic Left Hepatatectomy Using the Caudal Approach. https://vimeo.com/199911532. Feb 2017.