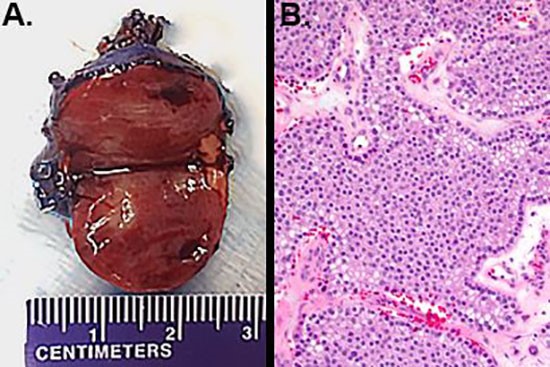
Figure 3. a) Gross pathology demonstrated a 2.6 cm parathyroid tumor. b) On hematoxylin and eosin staining, the parathyroid tumor was hypercellular, with decreased intracellular fat. No rim of normal parathyroid tissue was identified (200 X magnification).
Discussion
PHPT is the most common cause of hypercalcemia in the ambulatory population.1 The incidence varies widely, from 0.4 to 21.6 cases per 100,000 adults annually.2,3 Elderly females are two to three times more likely to be affected.4 The causative entity of PHPT is most commonly a single parathyroid adenoma in 80%–85% of patients; multi-gland parathyroid disease constitutes a further 15% of cases, with parathyroid carcinoma contributing approximately 1% of cases.5 Although PHPT is sporadic in >95% of cases, germline mutations in MEN1, and HRPT2 are associated with the familial PHPT syndromes of multiple endocrine neoplasia types 1 and 2A, and the hyperparathyroidism jaw-tumor syndrome, respectively.6 In patients with familial syndromes, a higher suspicion for multi-gland disease may exist. Parathyroidectomy remains the only definitive therapy for PHPT, and bilateral exploration should be performed for patients in whom multi-gland disease is suspected.
Approximately 1.6%–6% of patients with PHPT present with hypercalcemic crisis.7,8 Hypercalcemic crisis is variably defined as an adjusted serum calcium level of >13.5–14 mg/dL, with accompanying signs and symptoms of hypercalcemia.8 Of PHPT patients presenting in hypercalcemic crisis, the underlying pathology is found to be parathyroid adenoma in 85%–88%; multi-gland disease in 5%–10%, parathyroid cyst in 0%–5%; and parathyroid carcinoma in 4.5%–5%.8 Some authors suggest that a microcystic histologic pattern may correlate with hypercalcemic crisis in patients with parathyroid adenomas.7 Treatment of hypercalcemic crisis includes intravenous fluid resuscitation, judicious use of loop diuretics once volume repletion has been achieved, bisphosphonates, and dialysis when other modalities fail.8,9 Thiazide diuretics are contraindicated in the treatment of hypercalcemia, as they enhance calcium reabsorption in the distal tubule. With a rapid onset of action, calcitonin is a valuable adjunct to bisphosphonate therapy.9 Once medical stabilization has been achieved, early surgery constitutes definitive management and is highly successful.10,11 Traditional management consisted of emergency surgery within 24–72 hours; however this was associated with a high mortality rate.12 Improved medical control of hypercalcemia with intravascular fluid repletion, bisphosphonates, and correction of electrolyte imbalances may stabilize patients for surgery and help prevent life-threatening arrhythmias.8 The long lasting effects of bisphosphonates (2–12 weeks in the case of pamidronate) may contribute to the potential for postoperative hypocalcemia, underscoring the importance of close sequential monitoring after surgery.
Although hypercalcemic crisis raises clinical suspicion for parathyroid carcinoma, primary parathyroid malignancy remains an uncommon cause of hypercalcemic crisis.13 Current guidelines of the American Association of Endocrine Surgeons suggest that a diagnosis of parathyroid carcinoma be considered in patients with primary hyperparathyroidism with markedly elevated serum calcium and PTH levels.5 Although diagnosis of parathyroid carcinoma is made histologically, preoperative imaging demonstrating invasion of the thyroid or other adjacent structures might raise suspicion for carcinoma. No evidence-based guidelines exist for the preoperative evaluation of suspected parathyroid carcinoma, but cross-sectional imaging such as CT or MRI might provide additional anatomic information in cases where sonographic evaluation is equivocal or suspicious. Intraoperative findings of a white or gray, firm, fixed, adherent or fibrotic mass would raise suspicion for a parathyroid carcinoma. Suggested operative management (if there is intraoperative suspicion for parathyroid carcinoma) includes complete resection of the parathyroid tumor with avoidance of capsular disruption, to prevent subsequent parathyromatosis. En bloc resection of adherent tissues, including adjacent thyroid gland, may improve the likelihood of cure if cancer is confirmed histologically.
Hungry bone syndrome is a postoperative complication encountered most commonly in patients with preexisting bone disease, and renal failure.14 After parathyroidectomy, the abrupt decrease in PTH levels leads to a net influx of calcium, phosphate, and magnesium into bone, causing hungry bone syndrome. This manifests in electrolyte imbalances which may require frequent monitoring and intravenous repletion or dialysis to prevent neuromuscular and cardiac dysfunction.
Conclusion
PHPT is the most common cause of hypercalcemia in the nonhospitalized population. Hypercalcemic crisis is an uncommon presentation of PHPT. Although markedly elevated serum calcium and PTH levels raise clinical suspicion for parathyroid carcinoma, parathyroid adenoma remains the most common cause of both PHPT and PHPT presenting as hypercalcemic crisis. Mainstays of treatment of hypercalcemic crisis include intravenous fluids, induced calciuresis, bisphosphonates, calcitonin, and dialysis. Surgical resection remains the only definitive therapy for PHPT, and expeditious surgery after medical stabilization is recommended for patients presenting in hypercalcemic crisis.
Lessons Learned
Hypercalcemic crisis is an uncommon presentation of primary hyperparathyroidism. The differential diagnosis includes parathyroid adenoma, multi-gland hyperplasia, parathyroid cyst, and parathyroid carcinoma. Initial treatment should focus on management of hypercalcemia with fluid repletion, loop diuretics, intravenous bisphosphonates, and dialysis. Surgical resection represents definitive management, and should not be delayed.
Authors
Wachtel Ha,c, Sadow PM, MD, PhDb,c, Phitayakorn Ra,c, Parangi Sa,c
Correspondence Author
Sareh Parangi, MD, FACS
Massachusetts General Hospital
15 Parkman Street, Wang ACC 460
Boston, MA 02114
617-643-7935
sparangi@partners.org
Author Affiliations
- Massachusetts General Hospital, Dept. of Surgery, Div. of General & Endocrine Surgery, Boston, MA
- Massachusetts General Hospital, Dept. of Pathology, Boston, MA
- Harvard Medical School, Boston, MA
References
- Kinder BK, Stewart AF. Hypercalcemia. Curr Probl Surg. 2002;39:349-448.
- Wermers RA, Khosla S, Atkinson EJ, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993-2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006;21:171-7.
- Yu N, Donnan PT, Murphy MJ, Leese GP. Epidemiology of primary hyperparathyroidism in Tayside, Scotland, UK. Clin Endocrinol. 2009;71:485-93.
- Fraser WD. Hyperparathyroidism. Lancet (London, England). 2009;374:145-58.
- Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016;151:959-68.
- Sharretts JM, Simonds WF. Clinical and molecular genetics of parathyroid neoplasms. Best Pract Res Clin Endocrinol Metab. 2010 Jun;24(3):491-502. doi: 10.1016/j.beem.2010.01.003.
- Starker LF, Bjorklund P, Theoharis C, Long WD, 3rd, Carling T, Udelsman R. Clinical and histopathological characteristics of hyperparathyroidism-induced hypercalcemic crisis. World J Surg. 2011;35:331-5.
- Phitayakorn R, McHenry CR. Hyperparathyroid crisis: use of bisphosphonates as a bridge to parathyroidectomy. J Am Coll Surg. 2008;206:1106-15.
- Ahmad S, Kuraganti G, Steenkamp D. Hypercalcemic crisis: a clinical review. Am J Med. 2015;128:239-45.
- Lew JI, Solorzano CC, Irvin GL, 3rd. Long-term results of parathyroidectomy for hypercalcemic crisis. Arch Surg. 2006 Jul;141(7):696-9; discussion 700.
- Beck W, Lew JI, Solorzano CC. Hypercalcemic crisis in the era of targeted parathyroidectomy. J Surg Res. 2011;171:404-8.
- Ziegler R. Hypercalcemic crisis. J Am Soc Nephrol. 2001 Feb;12 Suppl 17:S3-9.
- Cannon J, Lew JI, Solorzano CC. Parathyroidectomy for hypercalcemic crisis: 40 years' experience and long-term outcomes. Surgery. 2010;148:807-12; discussion 12-3.
- Shindo M, Lee JA, Lubitz CC, et al. The Changing Landscape of Primary, Secondary, and Tertiary Hyperparathyroidism: Highlights from the American College of Surgeons Panel, "What's New for the Surgeon Caring for Patients with Hyperparathyroidism". J Am Coll Surg. 2016;222:1240-50.