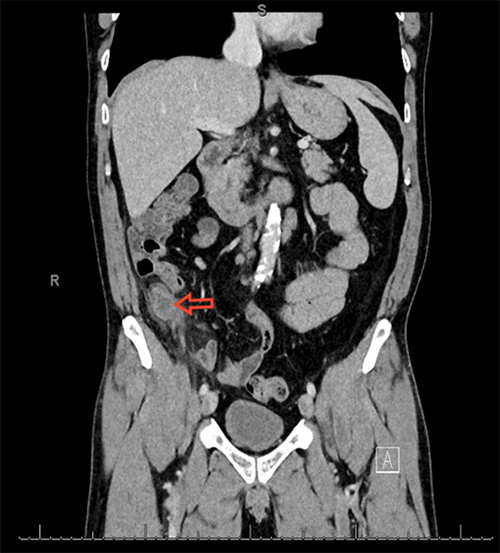
Figure 11. Six months postoperative pictures of syndactyly repair of 1st web space.
Discussion
Syndactyly is the most common congenital hand anomalies.1 A few associated congenital diseases associated with syndactyly are acrosyndactyly, Poland syndrome, Apert syndrome, and Carpenter syndrome.
Syndactyly is typically classified as simple, complex, complicated, incomplete, or complete. Simple syndactyly is denoted by only soft tissue involvement in the formation of the web. Complex syndactyly indicates some form of osseous fusion involved. Complicated syndactyly was used to denote multiple bony fusions or other skeletal abnormalities such as polydactyly or brachydactyly.9 Incomplete versus complete syndactyly is used to denote whether the soft tissue fusion extends to the finger tips. Flatt’s classification system was denoted by Type A (complete) and Type B (incomplete).
Syndactyly has been traditionally treated with operative release during the first years of life.7,13 The potential severe complications from this release are web creep, hyperpigmentation, donor site morbidity, contractors, and hypertrophic scarring.6,8
When the surgery is performed, there is usually a deficit of skin for coverage of the separated digits. Currently, there are two schools of thought as to how to perform the syndactyly release as to deal with this issue. One trend is to use full- or split-thickness skin grafts or some form of dermal substitute to make up the deficit.11,12 The oldest technique for syndactyly release was a zig zag incision pattern with a full thickness skin graft.13,17 There have been many different methods described for how to accomplish this while trying to minimize web creep and hypertrophic scars.10 A well-known full thickness skin graft technique created by Flatt10 was among them.
Various techniques surfaced capitalizing on the abundance of skin on the dorsal side of the hand to create a tri-lobed flap,18,19 bi-lobed flap15, and many other modifications which work well for incomplete simple syndactyly repair.16
Over the last two year period, the senior author has modified his technique for the repair of syndactyly to develop a unique procedure. Our initial experience with six syndactyly repairs, has been very encouraging. The syndactyly deformities repaired include simple, complicated, incomplete, and complete. The mean operative time was 75 minutes. The patients are discharged home the same day and are followed in the clinic at one week. Postoperatively, only one patient had a mild cellulitis of one side of the skin grafted site that responded to antibiotics. This patient had a complex complete syndactyly with a bony synostosis. We had no reoperations or web creep or any scar contractures. The follow up ranged from three months to 21 months. We recently performed a syndactyly repair of the toes with the same technique and the results have been satisfactory.
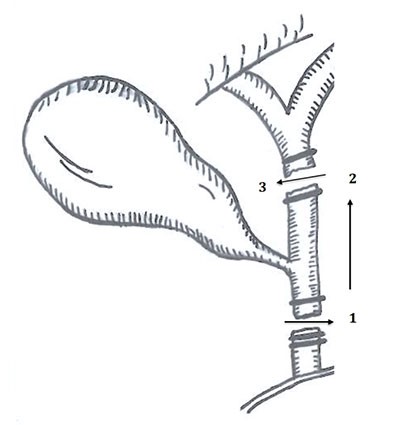
The technique itself is straight forward, and the end result of the surgery is promising; functionally and aesthetically. Full thickness skin grafts are used in all cases for the coverage of the raw surfaces which provides an excellent closure with minimal risk of secondary contracture. The salient features of our technique are: (1) A long dorsal skin flap, (2) Separation of the digits in a straight line; (3) Full thickness skin grafts to cover the raw surface.
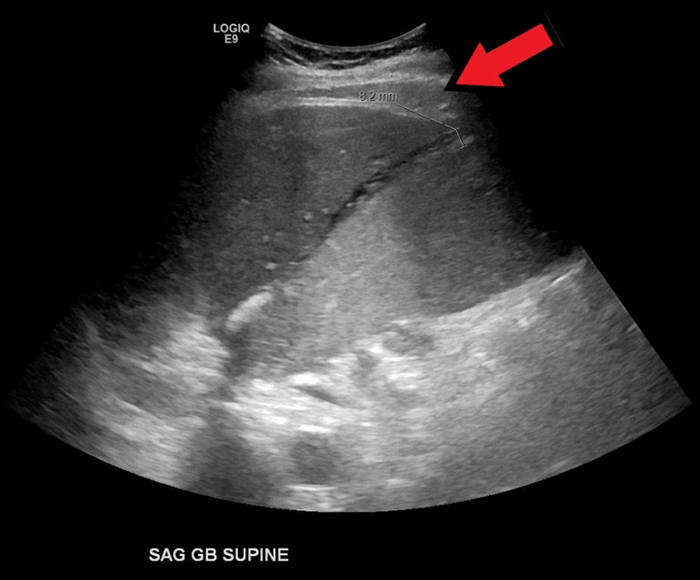
The operative markings: the dorsal flap is a rectangular flap that starts at the Metacarpo-Phalangeal joint of the involved digits and extends along the ray of the proximal phalanx just proximal to the PIP joints of the webbed digits. There is a slight concavity of the flap as it extends from proximal to the distal aspect. A straight line is marked in between the webbed fingers starting from the tip of the dorsal flap distally and extends all the way in between the webbed fingers across the dorsal aspect and extends to the palmar aspect of the web where it connects into the middle of the palmar incision. The palmar incision mark is placed corresponding to the level of the metacarpal heads on the palmar aspect.
The marked lines are incised; a thick dorsal flap is carefully dissected; the neurovascular structures are preserved ; the straight-line incision is then made up to the palmar horizontal incision, then the horizontal incision is completed; the dorsal flap is inset onto the palmar incision; the raw surface is measured on the longer finger; and a full thickness skin graft of double the dimensions is harvested from the groin site. The graft is defatted and inset snuggly on the raw surfaces with absorbable suture.
A bulky soft dressing is applied up to the elbow joint. The first dressing is changed in clinic at one week postop. At two weeks postop, the dressing is converted to a dry dressing as needed.
Conclusion
Multiple varieties of flap designs have been described and been proven successful in the creation of a web space for syndactyly repairs. The goal is to create a web space with near normal anatomic depth and to improve the function and dexterity of the hand as a unit, which our technique reliably achieves. The technique is simple in design and execution. The technique is easy to reproduce and teach. The usage of full thickness skin graft in all cases helps prevent any secondary contractures. Our preliminary results so far have been encouraging. Continued follow-up of these initial cases will help to confirm the benefits of this novel modification for syndactyly repair.
Lessons Learned
The straight-line technique with a full thickness skin graft shows promise as a simple, easy-to-learn procedure to correct hand and foot syndactyly with low incidence of complications like web creep, flexion contractures, or hypertrophic scar formation.
Authors
Gundlapalli V, Synovec J, Armstrong M
Correspondence Author
Vinay Gundlapalli
Plastic and Reconstructive Surgery
96 Jonathan Lucas St.
MSC 613/CSB 404
Charleston, SC 29425-6130
843-792-6228
vinaygsagar@gmail.com
Author Affiliations
Medical University of South Carolina
Division of Plastic Surgery
Charleston, SC 29425
Meeting Presentation
2016 American Society for Surgery of the Hand, Austin, TX, September 29–October 1, 2016
References
- Hovius, SE. Congenital hand IV: disorders of differentiation and duplication. In: Neligan PC, ed. Plastic Surgery. 3rd ed. Philadelphia, PA: Elsevier; 2012:603-633.
- Koskimies E, Lindfors N, Gissler M, Peltonen J, Nietosvaara Y. Congenital upper limb deficiencies and associated malformations in Finland: a population-based study. J Hand Surg Am. 2011;36(6):1058-1065
- Ekblom AG, Laurell T, Arner M. Epidemiology of congenital upper limb anomalies in 562 children born in 1997 to 2007: a total population study from Stockholm, Sweden. J Hand Surg Am. 2010;35(11):1742-1754.
- Kettelkamp DB, Flatt AE. An evaluation of syndactylia repair. Surg Gynecol Obster. 1961; 113:471-478
- Sari E. Analysis of web height ratios according to age and sex. J Plast Surg Hand Surg. 2015; 49:160-165
- Toledo LC, Ger E. Evaluation of operative treatment of syndactyly. J Hand Sug Am. 1979;4(6):556-564
- Hajnis K. Growth of the fingers and periods suited for operation on their congenital defects. Acta Chir Plast. 1968;10:267-284
- Dao KD, Shin AY, Billings A, Oberg KC, Wood VE. Surgical treatment of congenital syndactyly of the hand. Am Acad Orthop Surg. 2004; 12:39-48
- Kay SP. Syndactyly. In: Green DP, Hotchkiss RM, Pederson WC, et al, editors. Green’s operative hand surgery, 5th ed. Philadelphia, PA: Elsevier Churchill Livingstone. 2005; 1381-1391.
- Van der Biezen JJ, Bloem JJ. Dividing the fingers in congenital syndactyly release: a review of more than 200 years of surgical treatment. Ann Plast Surg. 1994; Aug: 33(2):225-230.
- Duteille F. Truffandier MV, Perrot P. Matriderm dermal substitute with split-thickness skin graft compared with full-thickness skin graft for coverage of skin defects after surgical treatment of congenital syndactyly: result in 40 commissures. J Hand Surg Eur. 2016; 41:350-351.
- Landi A, Garagnani L, Leti Acciaro A, Lando M. Ozben H, Gagliano MC. Hyaluronic acid scaffold for skin defects in congenital syndactyly release surgery: a novel technique based on the regenerative model. J Hand Surg Eur. 2014; 39:994-1000.
- Bauer T, Tondra J, Trusler H. Technical Modification in Repair of Syndactylism. Plast and Recon Surg. 1956; 17(5):385-392.
- Flatt AE. The care of congenital hand anomalies, 2nd Edn. St. Louis, Quality Medical Publishing. 1994: 228-275.
- Sahin C, Ergun O, Kulahci Y, et al. Bilobed flap for web reconstruction in adult syndactyly release: a new technique that can avoid the use of skin graft. J Plast Recon Aesth Surg. 2014; 67:815-821
- Single-Stage Separation of 3- and 4-Finger Incomplete Simple Syndactyly With Contiguous Gull Wing Flaps: A Technique to Minimize or Avoid Skin Grafting. Xiaofei Tian, MD, Jun Xiao, MD, Tianwu Li, MD, Wei Chen, MD, Qiu Lin, MD, Harvey Chim, MD. J Hand Surg Am. 2017;42(4):257-264.
- Karamese M, Akdag O, Selimoglu MN, Unal Yıldıran G, Tosun Z.V-Y and rectangular flap combination for syndactyly repair. J Plast Surg Hand Surg. 2016;50(2):102-6. doi: 10.3109/2000656X.2015.1106409. Epub 2015 Nov 5.
- Ekerot L. Syndactyly correction without skin grafting. J Hand Surg 1996; 21B: 330–337.
- Niranjan NS, Azad SM, Fleming AN, Liew SH. Long-term results of primary syndactyly correction by the trilobed flap technique. Br J Plast Surg. 2005 Jan;58(1):14-21.
- Wafa AM. Hourglass dorsal metacarpal island flap: a new design for syndactylized web reconstruction. J Hand Surg Am. 2008 Jul-Aug;33(6):905-8.
- Sherif MM. V-Y dorsal metacarpal flap: a new technique for the correction of syndactyly without skin graft. Plast Reconstr Surg. 1998 Jun;101(7):1861-6.