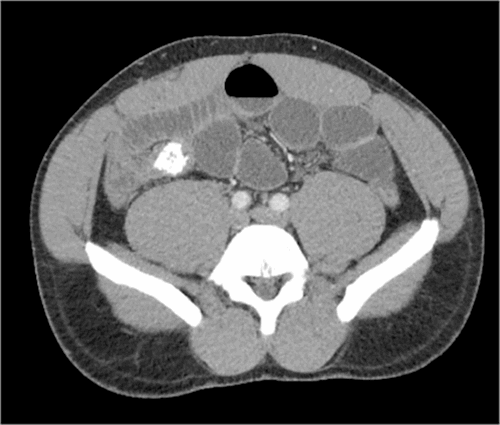
Figure 6. Extracted bullet.
The back of the heart was examined and there was no compromise of the epicardial surface. The septal defect and atriotomy were closed and the patient was rewarmed. The patient weaned off cardiopulmonary bypass without issue. Postoperative transesophageal echocardiogram demonstrated good LV and mitral valve function. The patient was extubated and transferred to the cardiovascular intensive care unit (CICU) for recovery.
The patient remained in the CICU postoperatively for two days without the need for inotropic support. He was discharged home on postoperative day three. Antibiotics for bacterial endocarditis prophylaxis were given for six months.
Discussion
We report a rare case of an NPG injury that highlights the importance of considering NPGs to be dangerous and capable of causing life-threatening or fatal injuries similar to those caused by more traditional firearms. Although our patient presented in stable condition, the pellet could have easily caused significant pulmonary and cardiac injury, with plausible presentations ranging from arrhythmias to pericardial effusion with tamponade or massive hemorrhage and death. It is well known that once a bullet hits the body, it can travel in any direction at different speeds depending on the characteristics of the mass in the body tissue. In this present case, the bullet entered a vessel and its path was redirected with significant force to penetrate the myocardium. The potential damage of these bullets should not be underestimated since, as seen in this case, they are able to travel unimaginable pathways with force. On the original report from EMS, the family was not going to bring the patient to the hospital; however the EMS personnel appropriately followed the penetrating injury protocol per trauma guidelines.
NPGs use air or another compressed gas type to propel an object.1 More than 60% (over 20,000 cases) of nonpowder gun injuries reported annually are in pediatric patients.2-3 Pediatric patients can have more significant injury due to their thin soft tissue coverage that is easily penetrable.1 Technology offers faster and more powerful NPGs, with muzzle velocities ranging from 290 to 940 feet/second.1,4 The critical velocity for penetration of human skin by an air gun pellet was found to be between 38-70 meters/second (125 +/ 230 feet/second)5 Air guns are not legally considered firearms; however, many have velocities that exceed some conventional handguns.4,6
Most NPGs do not require a license and are easily accessible to children due to these devices generally being considered safe.
1,4,7Case reports have shown that injuries from NPGs can be serious and sometimes fatal.
8-11The majority are accidental, and teenage patients are the most common victims; the most common sites of injury reported are the child’s head, eyes, neck, extremities, and thorax.
1,10-12Thoracic injuries from air guns can range from insignificant superficial injury to death.
4,6,8,11,13-15Conclusion
Despite the positive outcome of our patient, serious injuries by NPGs have led to significant morbidity in the pediatric population. Previous cases reports have indicated that underestimating potentially serious injuries by NPGs have led to fatal outcomes.6
Lessons Learned
Although NPGs injuries are rare, they can cause significant harm. The legal nature of NPGs may mislead children and their caregivers into considering these devices to be safe. Muzzle velocities have impressively increased and the accessibility of these devices should therefore be revised.
Authors
Gurria Ja, Riney Lb, Fain Ec, Brown Rd, Morales De
Correspondence Author
Juan Gurria, MD
Division of Pediatric General and Thoracic Surgery
Trauma Surgery Fellow
Cincinnati Children’s Hospital Medical Center
3333 Burnet Ave.
ML 2023
Cincinnati, OH 45229
713-291-6850
Juan.Gurria@cchmc.org
Author Affiliations
- Cincinnati Children’s Hospital Medical Center, Division of Pediatric General and Thoracic Surgery, Cincinnati, OH
- Cincinnati Children’s Hospital Medical Center, Division of Emergency Medicine, Cincinnati, OH
- Cincinnati Children’s Hospital Medical Center, Division of Emergency Medicine, Cincinnati, OH
- Cincinnati Children’s Hospital Medical Center, University of Cincinnati Department of Surgery, Cincinnati, OH
- Clark-Helmsworth Chair of Pediatric Cardiothoracic Surgery, Heart Institute Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, OH
References
- Khan UU, Kamal N, Mirza S, Sherief L. Pediatric air gun shot injury. Saudi Med J. 2014;35(12): 1507-9.
- Scribano PV, Nance M, Reilly P. Pediatric nonpowder firearm injuries: outcomes in an urban pediatric setting. Pediatrics. 1997;100(4):E5.
- Centers for Disease Control and Prevention (CDC). BB and pellet gun-related injuries--United States, June 1992-May 1994. MMWR Morb Mortal Wkly Rep. 1995;44(49):909-13.
- Isik O, Engin C, Daylan A, Sahutoglu C, Air gun pellet: cardiac penetration and peripheral embolization. Ulus Travma Acil Cerrahi Derg. 2016;22(3):301-3.
- DiMaio VJ. Penetration and perforation of skin by bullets and missiles. A review of the literature. Am J Forensic Med Pathol. 1981 ;2(2):107-10.
- Misseldine S, August DA. Anesthesia for a thoracic BB gun injury. Paediatr Anaesth. 2010;20(6):566-73.
- Wightman G, Cochrane R, Gray R, Linton M. A contribution to the discussion on the safety of air weapons. Sci Justice. 2013;53(3):343-9.
- DeCou JM, Abrams R, Miller R. Life-threatening air rifle injuries to the heart in three boys. J Pediatr Surg. 2000;35(5):785-7.
- Milroy CM, Clark J, Carter N. Air weapon fatalities. J Clin Pathol. 1998;51(7):525-9.
- Klein JA, Nowak J, Sutherell J, Wheeler D. Nonsurgical management of cardiac missiles. Pediatr Emerg Care. 2010;26(1):36-8.
- Bakovic M, Petrovecki V, Strinovic D, Mayer D. Shot through the heart-firepower and potential lethality of air weapons. J Forensic Sci. 2014;59(6):1658-61.
- Navarro-Mingorance A, Reyes-Dominguez SB, Leon-Leon MC. Pediatric orbital emphysema caused by a compressed-air pistol shot: a case report. Arch Soc Esp Oftalmol. 2014;89(9):373-5.
- Nakamura DS, McNamara J, Sanderson L. Thoracic air gun injuries in children. Am J Surg. 1983;146(1):39-42.
- Hudson AJ Wyatt JP. Cardiac air gun pellet injury. Emerg Med J. 2001;18(6):519.
- Alejandro KV, Acosta JA, Rodriguez PA. Air gun pellet cardiac injuries: case report and review of the literature. J Trauma. 2003;54(6):1242-4.