Figure 1. MRI of abdomen and pelvis showing a 2 x 3 cm mass at the hepatic hilum and surrounded by an 8 x 12 cm hematoma. Coronal (SUB_COR Post) view.
After initially refusing surgical intervention, the patient was transferred to our tertiary center three months later for evaluation where she complained of worsening symptoms, in addition to, loss of appetite and lower extremity swelling. At that time, her laboratory results demonstrated a normal CBC, total bilirubin was 6.7, CEA was 0.9, CA 19-9 was 1788, alkaline phosphatase was 488, AST 237, and ALT 30 and chest XR with no evidence of metastatic lesions. Her cancer antigen 19-9 was also elevated at 1788 U/mL. On exam, she was noted to be thin, no hepatic encephalopathy, jaundiced with scleral icterus, non-tender abdomen with no palpable masses or ascites noted. A repeat MRI abdomen/pelvis was performed demonstrating an overall unchanged appearance of the previous hemorrhagic hilar “cholangiocarcinoma,” but now with extension of the hematoma to segment 4 and liver hilum was seen, measuring 12.4 cm in total. The mass was causing severe intrahepatic duct dilation of the central and left intrahepatic ducts due to mass effect and obstruction at the distal hepatic hilum and mass effect on the intrahepatic IVC and portal vein but both vessels remained patent. In addition, there also was evidence of cholangitis.
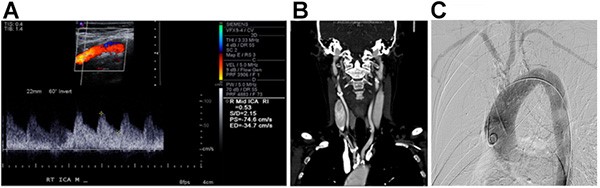
During the patient’s first admission, she was found to be cholangitic with a bilirubin of 24, an elevated WBC and fevers. Gastroenterology (GI) performed an endoscopic ultrasound (EUS) with FNA of the mass in addition to direct visualization of the biliary tree with a fiberoptic camera and endoscopic retrograde cholangiopancreatography (ERCP) with placement of a 10 French biliary stent into the common bile duct and extending into the right hepatic duct. They noted a submucosal mass with blood clot in the main bile duct at the takeoff of the right hepatic duct. Brushings and biopsies of the mass were taken during the ERCP and found to be negative for malignancy. The left hepatic duct was not able to be opacificed due to obstruction.
Her cholangitis resolved and her bilirubin down trended. The patient was sent home with a percutaneous transhepatic catheter (PTC) drain in place with plans to follow up as an outpatient regarding surgical planning for an extended right hepatectomy once she recovered from her infection. She was readmitted several times with cholangitis, treated and sent home to improve her nutrition with plans for eventual surgery. An additional repeat MRI abdomen/pelvis was performed and noted to have interval progression of cholangiohepatitis of the right hepatic lobe with development of approximately ten cholangitic abscesses, with the largest measuring 2.5 cm. The complex hematoma encased mass at the hepatic hilum continued to demonstrate further interval increase in size with the hematoma now exerting increased mass effect at the left hepatic lobe.
After failed preoperative nutritional optimization and resolution of cholangitis, she was taken to the operating room for a diagnostic laparoscopy, which did not demonstrate any carcinomatosis or obvious peritoneal metastasis. We proceeded with the planned, open extended right hepatectomy in order to achieve an en bloc resection of tumor mass with a liver remnant of 30 percent. Intraoperatively, it was noted that the tumor mass and hematoma was confined to the liver but there was desmoplastic change adherent to the first portion of the duodenum.
Her surgical pathology revealed a 12 cm x 11 cm x 6.5 cm high grade, undifferentiated pleomorphic sarcoma with the hilar margin and gallbladder fossa positive for sarcoma, 0/2 lymph nodes positive, mitotic rate of 2/10 in high power field with positive lymphovascular invasion and greater than 40 percent tumor necrosis. A peritoneal nodule was also biopsied during surgery and found to be positive for sarcoma on final pathology. Based on pathological staging, she was a pT2bN0M1, consistent with Stage four undifferentiated pleomorphic sarcoma. According the French Federation of Cancer Centers Sarcoma Group grading system, this patient’s cancer was determined to be a Grade 3 sarcoma.
The patient had a prolonged postoperative course in the hospital and was discharged home with her family on postoperative day 60. The patient did however succumb to her disease shortly afterwards.
Discussion
Pleomorphic Sarcoma of the liver is a rare disease that is still poorly understood, but the limited data from large cancer centers are encouraging. Despite our patient’s outcome, we believe that based upon her Palliative performance scale score and her recurrent infections that she deserved a chance for surgical palliation. Palliative surgery has proven to benefit patients that are strong surgical candidates, which is directly correlated with: life expectancy, lifestyle, and overall health. Patients who present as strong surgical candidates can benefit in terms of comfort, wound healing, and prolonged life expectancy.3
This patient was not a strong surgical candidate based upon her poor nutritional status and the size of the mass, however the lack of a preoperative tissue diagnosis, the recurrent infections, and the patient’s motivation made a case for surgical palliation. Preoperative nutrition optimization failed due to the combination of factors. The patient initially refused nasogastric feeds and was continuously catabolic given the malignancy and recurrent bouts of cholangitis. Also, it was important for the patient to return home, which was about 300 miles away. However, we believe that if the patient had stayed closer to the hospital, that we may have been more successful with nutritional optimization and biliary drainage. Our operative team realized that these were not optimal conditions, but given a lack of tissue diagnoses, we retained some small hope that the increased size of the mass represented peri-tumor hematoma as opposed to cystic expansion of the malignancy and that a palliative resection could still improve her quality of life.
Prognosis of UPS is often poor regardless of intervention. Prognosis is often based upon size and staging of the primary UPS.4 On the basis of a prospectively followed cohort of adult patients with primary soft tissue sarcoma (STS) who were treated at Memorial Sloan-Kettering Cancer Center, a nomogram for predicting sarcoma-specific mortality at 12 years was developed.4 Nomogram predictor variables included age at diagnosis, tumor size (<or =5, 5 to 10, or >10 cm), histologic grade (high or low), histologic subtype (fibrosarcoma, leiomyosarcoma, liposarcoma, malignant fibrous histiocytoma, malignant peripheral nerve tumor, synovial, or other), depth (superficial or deep), and site (upper extremity, lower extremity, visceral, thoracic or trunk, retrointraabdominal, or head or neck. The accuracy of the nomogram has been validated by both internal and external standards. The tool is meant to be used in adult patients who are less than six months from their index surgical procedure and are without evidence of metastatic disease. The sarcoma nomogram may be useful for patient counseling, follow-up scheduling, and clinical trial eligibility determination.
Thus, due to the rapid growth of the mass in a relatively short amount of time, the failed nutritional optimization and increasing frequency of hospitalizations, it was unlikely that surgical resection (three months after presentation) would improve prognosis of the patient, but we hoped that it would improve the quality of her remaining days. Challenges in this particular case included poor nutritional status recalcitrant to nutritional adjuncts, social issues (family opposed patient’s election for surgery), and logistically the patient lived far from the hospital (300 miles).
In conjunction with the increasing size of the mass as well as the overall health of the patient at that time, surgery was suboptimal. In retrospect, since growth can occur rapidly depending on the subcategory of primary UPS, our patient may have had a better outcome with a lower threshold for surgical intervention.
Conclusion
Low grade, small, UPS of the liver should absolutely be resected with curative intent. However, challenges remain concerning the best course of palliation for those patients with larger UPS of the liver. Patient motivation, nutrition and biliary patency weigh heavily on hepatic UPS palliation. In conclusion, for lesions larger than 10 cm, we would encourage a brief trial of nutritional adjuncts limited to no more than two weeks and if there are no objective signs of nutritional improvement, the decision to operate or not to operate should be finalized.
Lessons Learned
Undifferentiated pleomorphic sarcoma (UPS) of the liver is a rare and challenging disease that requires an understanding of the progression and presentation of the disease as well as the patients’ background. Palliative surgery and care are important considerations for UPS. This literature review is intended to expand on the current research in order to facilitate an improved understanding of UPS.
Authors
Dishong I, Lee E, Rankin TM, Jie T
Correspondence Author
Timothy Rankin, MD, MS
University of Arizona College of Medicine
1501 N. Campbell Ave. Suite 4402
Tucson, AZ 85724
949-573-3368
tmrankin.md@gmail.com
Author Affiliations
University of Arizona
Department of Surgery
Tucson, AZ
References
- Toro JR, Travis LB, Wu HJ, et al., Incidence patterns of soft tissue sarcomas, regardless of primary site, in the surveillance, epidemiology and end results program, 1978-2001: An analysis of 26,758 cases. Int J Cancer, 2006. 119(12): p. 2922-30.
- Ye MF, Zheng S, Xu JH, et al., Primary hepatic malignant fibrous histiocytoma: a case report and review of the literature. Histol Histopathol, 2007. 22(12): p. 1337-42.
- Rankin T, Mailey B, Suliman A, et al., Palliative reconstructive surgery may improve quality of life in high functioning noncurable head and neck oncologic patients. Ann Plast Surg, 2015. 74 Suppl 1: p. S52-6.
- Kattan MW, Leung DH and Brennan MF. Postoperative nomogram for 12-year sarcoma-specific death. J Clin Oncol, 2002. 20(3): p. 791-6.