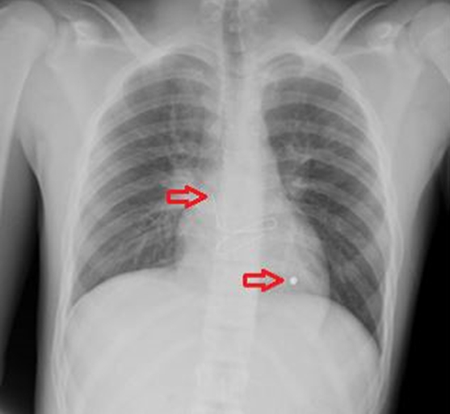
Figure 2. EUS revealed a 27 mm, hypoechoic, lobulated mass in the mid-body consistent with a uT2-3N0M0 tumor.
Although the EUS findings favored uT3 tumor, in certain planes of imaging the tumor also appeared consistent with a uT2 tumor. Biopsy was consistent with a well-differentiated adenocarcinoma. Metastatic workup, including a computed tomography CT of the chest/abdomen/pelvis and a positron emission tomography—computed tomography (PET/CT) were otherwise unremarkable. The patient underwent multidisciplinary evaluation and was discussed at our multidisciplinary gastrointestinal tumor board. Upon further review (including immunohistochemistry), the pathologist was unable to determine whether the adenocarcinoma represented a gastric primary or metastatic lesion from his colorectal cancer.
Based on the EUS findings and negative metastatic work-up, the group consensus was that this likely represented a primary gastric cancer. As such, the patient was taken to the operating room in November 2016. At exploration, there was no evidence of carcinomatosis or liver metastases. The mass was readily palpable in the gastric body, and the overlying serosa was intact and unremarkable. He therefore underwent an uncomplicated open subtotal gastrectomy with Roux-en-Y gastrojejunostomy and a modified D2 lymphadenectomy for a presumed primary gastric cancer. Final pathology, however, ultimately revealed a 2.5 cm adenocarcinoma which was morphologically identical to patient's colon primary. More specifically, immunohistochemical stains demonstrated that the tumor cells were positive for CK20, CDX2, and Villin and negative for CK7, consistent with the patient’s colon primary. Of note, the tumor invaded through the muscularis propria and into (but not through) the subserosa. There was no evidence of lymphovascular or perineural invasion, and all 17 harvested nodes were negative for tumor. The case was discussed at multidisciplinary cancer case conference; given that the sole site of colon cancer metastasis had been completed resected, the group consensus was that adjuvant therapy was not indicated.
Discussion
Gastric mucosal metastases, also known as “secondary gastric cancers”, are rare events. The incidence of mucosal metastases metastasis is difficult to assess since the majority of cases are found at autopsy, but literature suggests that it may range from 0.7-5.4 percent.1-3 The average age at diagnosis is 59.1 years (range 56 to 71 years), and the average time from diagnosis of the primary tumor to diagnosis of the secondary gastric cancer metastasis ranges from 16 to 78 months.4 Almost half of these patients present with additional metastases to other organs.5 According to Oda et al, cancers most frequently reported to metastasize to the gastric mucosa were melanoma (29.6 percent), breast (11.6 percent), esophageal (11.5 percent), lung (6.8 percent), thyroid (6.4 percent), and renal cell (6.2 percent).1 In another series, 27.9 percent of cases of gastric metastasis were due to breast cancer, followed by lung cancer (23.8 percent), esophageal cancer (19.1 percent), renal cell cancer (7.6 percent), and malignant melanoma (7 percent).4 Although the literature on gastric mucosal metastases is largely limited to case reports and small case series, general guidelines and potential pitfalls regarding work-up and treatment of these rare tumors can be gleaned from these reports.
Most patients with gastric mucosal metastases are asymptomatic at presentation (as evidenced by the fact that the majority are incidentally diagnosed at autopsy).1 Some patients, however, present with signs and symptoms consistent with primary gastric cancers, including anorexia, nausea, vomiting, abdominal pain, and weight loss, as well as acute upper gastrointestinal (GI) bleeding and/or iron-deficiency anemia.6 In a report by Kim et al of 37 patients with gastric mucosal metastases, occult or overt GI bleeding was the most common presentation (32.4 percent of cases).7 The first step in the diagnostic work-up of these symptomatic patients is EGD with biopsy.7 In some cases, pathologic evaluation of the gastric biopsy may be the first clue of an otherwise occult primary cancer.
At EGD, gastric mucosal metastases can usually be categorized into one of three categories based on their endoscopic features: non-ulcerated masses, submucosal masses with ulceration at their apex, or multiple nodules of varying sizes with ulceration.7,8 Some reports have described a characteristic “bull’s eye sign”, or a raised lesion with central depression.9,10 In a series from the National Cancer Center Hospital in Tokyo composed of 54 patients with gastric mucosal metastases and 347 autopsy cases, the majority of tumors were solitary (65 percent) versus multiple (35 percent).1 In addition, the majority of lesions were located in the middle or upper thirds of the stomach.1 Our patient had a solitary, fungating mass with a central depression located along the lesser curve in the mid-body. Lesions can also appear as polypoid masses ulcers, ulcerated protruding lesions, or thickening of the gastric wall.7,11 Of note, the primary tumor type may dictate the endoscopic features of the gastric mucosal metastasis. For example, gastric mucosal metastases from melanoma may appear as melanotic nodules or as masses with necrosis and melanosis on EGD.12
Patients with gastric mucosal metastases should be routinely discussed at multidisciplinary cancer case conference. Optimal treatment will vary based on the primary tumor type, symptoms at presentation, and the number of gastric metastases. In the case series reported by Kim et al, 23/37 cases (62.2 percent) presented with solitary lesions. Twelve of these patients received some form of treatment for their gastric metastasis. Surgical resection was performed in six patients, including partial gastrectomy alone in two patients with metastatic lung cancer, partial gastrectomy with adjuvant chemoradiation in two patients with metastatic esophageal cancer, wedge resection alone in a patient with metastatic renal cell carcinoma, and wedge resection with adjuvant chemotherapy in a patient with metastatic melanoma. The median overall survival inclusive of all 37 patients was 18.0 months (interquartile range (IQR), 6.0 to 18.0 months) after diagnosis of their primary cancer and 3.0 months (IQR, 1.0 to 11.0 months) after diagnosis of their secondary gastric cancer.7 The median overall survival in the 12 patients who were treated was longer than in patients who were not treated (11.0 months [IQR, 9.0 to 30.0 months] vs 2.0 months [IQR, 1.0 to 11.0 months; p<0.001]. In addition, the median overall survival of patients with solitary metastases was better than that of patients with multiple metastases (7.0 months [IQR, 2.0 to 13.0 months] vs 2.0 months [IQR, 1.0 to 6.0 months]; p=0.047). Although this case series was relatively small and case-selection bias may play a role, it suggests that patients with gastric mucosal metastases, particularly those with solitary lesions, may benefit from surgical resection.7
Heightened awareness of possible gastric mucosal metastases is warranted in cancer survivors with gastric symptoms noted during cancer surveillance or follow-up clinic visits, particularly in patients with a history of breast cancer, lung cancer, esophageal cancer, renal cell cancer, or melanoma. When caring for patients with possible gastric mucosal metastases, several steps should be followed to streamline and optimize care. In symptomatic patients, an EGD should be promptly performed and any abnormal appearing lesions should be biopsied. The gastroenterologist should be alerted to the possibility of gastric mucosal metastases and their characteristic features, such as a raised lesion with a central depression or submucosal masses with tip ulceration. The pathologist reviewing the case should be also alerted to the possibility of gastric mucosal metastases so that appropriate immunohistochemistry analyses are performed and biopsies are compared against slides from the patient’s original primary tumor. In our case, primary gastric adenocarcinoma was favored based on EUS findings, although metastatic colon cancer could not be rule out on pathologic review. Finally, all patients with possible gastric mucosal metastases should undergo multidisciplinary evaluation and be discussed at multidisciplinary cancer conference. In the setting of complete resection, routine use of adjuvant therapy is not recommended per National Comprehensive Cancer Network guidelines. These patients, however, are at high risk for future metastases; as such, close cancer surveillance is warranted.7
Conclusion
Gastric mucosal metastases are rare events. We present the case of a 71-year-old male who presented with a solitary colon metastasis to his gastric mucosa approximately three years after resection of his primary colon cancer and 2.5 years after partial left hepatic lobectomy for a previous hepatic colon metastasis. This report summarizes the limited literature currently available and discusses common presenting symptoms and diagnostic findings in patients with gastric mucosal metastases, as well as steps to optimize their workup and management.
Lessons Learned
Heightened awareness of possible gastric mucosal metastases is warranted in cancer survivors with gastric symptoms, particularly those with a history of melanoma, breast cancer, lung cancer, esophageal cancer, or renal cell cancer. EGD should be performed and any abnormal appearing lesions should be biopsied. The gastroenterologists and pathologists involved in the case should be alerted to the possibility of gastric mucosal metastases to ensure optimal endoscopic and pathologic evaluations, respectively. All patients with possible gastric mucosal metastases should undergo multidisciplinary evaluation and be discussed at multidisciplinary cancer conference. If appropriate, surgical resection should be considered, particularly in patients with symptomatic solitary lesions.
Authors
Goel N, Olszanski AJ, Esnaola NF
Correspondence Author
Neha Goel, MD
Department of Surgical Oncology
Fox Chase Cancer Center
333 Cottman Ave.
Philadelphia, PA 19111
neha.goel@fccc.edu
Author Affiliations
Departments of Surgical Oncology and Medical Oncology
Fox Chase Cancer Center
Philadelphia, PA
Disclosure of Conflicts
Dr. Goel has no conflicts of interest or financial disclosures to report. Dr. Olszanski has served as a consultant or advisor for Merck, Takeda, Bristol-Myers Squibb, Kyowa Hakko Kirin, and G1 Therapeutics. Dr. Esnaola has served as a consultant for Merck and Celgene.
References
- Oda I, Kondo H, Yamao T, et al. Metastatic Tumors to the Stomach: Analysis of 54 Patients Diagnosed at Endoscopy and 347 Autopsy Cases. Endoscopy. 2001;33(6):507–510.
- Palma GDD, Masone S, Rega M, et al. Metastatic tumors to the stomach: Clinical and endoscopic features. World J Gastroenterol. 2006;12(45):7326–7328.
- Kobayashi O, Murakami H, Yoshida T, et al. Clinical Diagnosis of Metastatic Gastric Tumors: Clinicopathologic Findings and Prognosis of Nine Patients in a Single Cancer Center. World J Surg. 2004;28(6).
- Namikawa T, Hanazaki K. Clinicopathological features and treatment outcomes of metastatic tumors in the stomach. Surgery Today. 2013;44(8):1392–1399.
- Campoli PMDO, Ejima FH, Cardoso DMM, et al. Metastatic cancer to the stomach. Gastric Cancer. 2006;9(1):19-25.
- Reiman T, Butts CA. Upper Gastrointestinal Bleeding as a Metastatic Manifestation of Breast Cancer: A Case Report and Review of the Literature. Canadian J of Gastroenterol. 2001;15(1):67–71.
- Kim GH, Ahn JY, Jung H-Y, et al. Clinical and Endoscopic Features of Metastatic Tumors in the Stomach. Gut and Liver. 2015;9(5).
- Hsu CC, Chen JJ, Changchien CS. Endoscopic Features of Metastatic Tumors in the Upper Gastrointestinal Tract. Endoscopy. 1996;28(02):249–253.
- Pomerantz H, Margolin HN. Metastases to gastrointestinal tract from malignant melanoma. Am J Roentgenol Radium Ther Nucl Med. 1962; 88:712–717.
- Richter R, Panish J, Berci G. Endoscopic findings in melanoma metastatic to the stomach. Gastrointest Endosc. 1972;18(4):172–173.
- Eivazi-Ziaei J, Esmaili H. Metastatic malignant melanoma affecting stomach. J Cancer Res Ther. 2014; 10(3): 733–736.
- Iconomou TG, Tsoutsos D, Frangia K, Gogas H, Papadopoulos S, Georgountzos V, Ioannovich J. Malignant melanoma of the stomach presenting with an unknown primary lesion. Eur J Plast Surg. 2003;26:153–155.