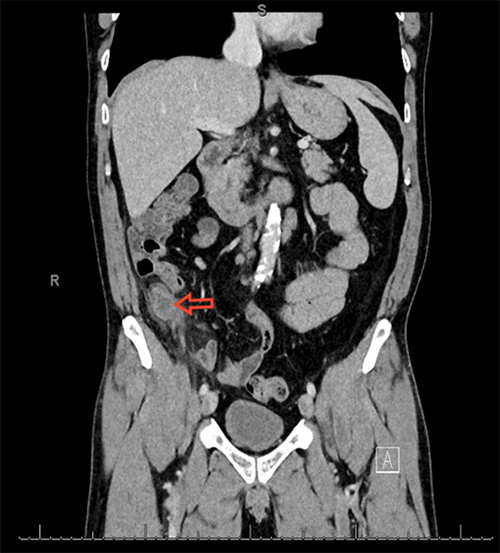
Figure 2. CT scan of abdomen done in ED on admission, lung window.
The differential diagnoses included: Ogilvie syndrome, volvulus, C. diff colitis or possibly a postpartum ischemic event. Surgery consulted OBGYN due to the unusual presentation so close to the delivery and performed an emergent exploratory laparotomy; the uterus was normal size for postpartum day five ruling out a uterine cause, such as infection, uterine perforation, etc. for the pneumoperitoneum. Upon further exploration, a perforated right colon, close to the hepatic flexure with fecal peritonitis was found. Due to the significant inflammation and peritonitis present, a clear etiology was not evident intraoperatively. Because of the patient’s instability, a quick but thorough inspection and palpation of the distal colon was done. There was no colonic redundancy to suggest volvulus. There were no gross tumors, any inflammation, or distension to suggest obstruction or infection. The rest of colon was seemingly very normal. A right hemicolectomy with anastomosis and diverting loop ileostomy was performed and two drains were left. The pathology workup of the specimen showed no abnormalities. One week postoperatively the patient had some fluid collections that could not be drained by interventional radiology and required an open washout with multiple drains placed. She recovered well and was subsequently discharged after ten days.
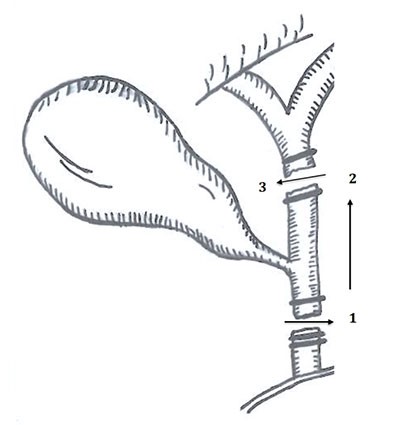
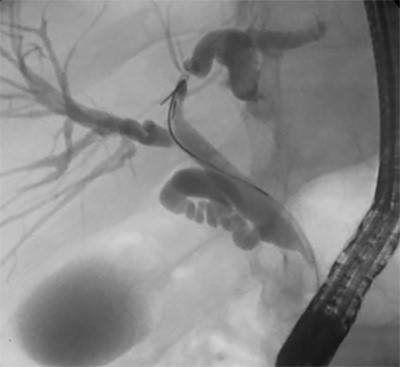
Her diverting loop ileostomy was reversed three months after discharge. The reversal was performed after thorough evaluation, including a barium enema and colonoscopy without any abnormal findings.
Discussion
A literature review over a three month period using many sources including but not limited to: DynaMed, New England Journal of Medicine, UpToDate, PubMed and Google scholar, revealed only three similar published cases of post-NVD bowel perforation; the latest of which was published in June 2014. All three aforementioned case reports cite Ogilvie syndrome as the cause of bowel perforation post-NVD.2,3 Ogilvie syndrome is a functional obstruction that can eventually progress to perforation, this can rarely present after a surgical procedure, such as a C-section. This presentation, though rare, is much more common than post-NVD. One published article describes post-NVD bowel perforation in a patient who had a significant history of symptomatic ulcerative colitis, including a previous proctocolectomy and ileo-pouch-anal anastomosis.4 The second case described an older patient who was having her second child via vaginal delivery.2 The third case is also an older woman post-NVD and her symptoms presented immediately after delivery of the fetus.3 Based on the aforementioned research, this is the first case report of its kind.
Our differential diagnoses for this patient included, C. diff colitis because of the antibiotic use before discharge due to a suspected urinary tract infection. A fecal leukocyte count was unremarkable, and stool C. diff PCR was negative. Volvulus was deemed unlikely during the surgery because the colon was not distended and no signs of volvulus were noted intraoperatively. Because of these findings, our working diagnosis was Ogilvie syndrome, pseudo obstruction complicated by ischemia and finally leading to right colon perforation. Ischemia complicates up to forty-two percent of all bowel obstructions (including patients not in the peripartum period) and significantly increases mortality and morbidity.1
The postpartum period can rarely lead to colonic pseudo obstruction of unclear etiology. This pseudo obstruction can lead to colonic dilation, ischemia of the bowel wall and eventually perforation. This disease process is very rarely found post-NVD. The etiology of Ogilvie syndrome is still unknown, but it has been known to occur with abdominal trauma, sepsis and abdominal or pelvic surgery. Making the diagnosis of Ogilvie syndrome is difficult because the symptoms are very nonspecific. The most common symptom noted in patients with Ogilvie syndrome is abdominal distension.1 One article reported that the association between Ogilvie syndrome and vaginal delivery maybe due to the declining serum estrogen levels in the postpartum period.5
Ogilvie syndrome that leads to perforation usually involves ischemia of the bowel wall. Other ischemia-related conditions can occur in the peripartum period due to a state of hypercoagulability during pregnancy. The most common ischemic event during the peripartum period is venous thromboembolism (VTE), this can occur anywhere, but commonly in the mesenteric, splenic, portal, pelvic and deep veins of the leg. Other postpartum ischemia-related conditions are: Sheehan syndrome, hypovolemic acute renal failure, ischemic heart disease and ischemic stroke.7 VTE in the postpartum period has a prevalence of 1 in 1600. Maternal deep vein thrombosis is more often associated with PE than as an isolated finding,8 PE is the seventh leading cause of maternal mortality (nine percent).9
The clinical signs of abdominal distension in the postpartum period should warrant a high suspicion for further evaluation despite these patients being generally healthy.
Conclusion
Colonic perforation is extremely rare in postpartum patients, but can happen, even in otherwise healthy women. The initial symptoms of abdominal distension and pain are vague, and sometimes expected in this population, but should raise consideration for further work-up or monitoring as the results can be devastating.
Lessons Learned
Postpartum patients with any abnormal abdominal distension or tenderness should be given a thorough evaluation. At the very least, these patients should have an abdominal x-ray performed and follow up if symptoms do not resolve clinically. This early diagnostic consideration will reduce morbidity and mortality for patients similar to the one presented in this case.
Authors
Laffoon AN, Knijnikov A
Correspondence Author
Allison Laffoon
335 Des Plaines Ave, Apt. G
Forest Park, IL 60130
712-251-9195
Allison.laffoon@gmail.com
Author Affiliations
West Suburban Medical Center
Department of Surgery
Oak Park, IL
References
- Bellary K. Spontaneous Caecal Perforation Associated with Ogilvie Syndrome Following Vaginal Delivery – A Case Report. J Clin Diagn Res. 2014;8(6):ND08-ND09. Doi: 10.7860/JCDR/2014/9078.4484
- Cartlidge D. Acute pseudo-obstruction of the large bowel with caecal perforation following normal vaginal delivery: a case report. J Med Case Rep. 2010;4:123. Doi: 10.1186/1752-1947-4-123
- Bhatti ABH. Acute colonic pseudo-obstruction after normal vaginal delivery. J Pak Med Assoc. 2010:19(30). http://www.jpma.org.pk/full_article_text.php?article_id=1930. Accessed May 10 2017.
- Spina V. Postpartum complications in a patient with a previous proctocolectomy and ileo-pouch-anal anastomosis for ulcerative colitis. J Prenat Med. 2012 Apr-Jun; 6(2):31-33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3421950/. Accessed May 11, 2017.
- >Strecker JR, Jaluvka V. Spontaneous caecum perforation following caesarean section. Geburtshilfe Frauenheilkd. PubMed. July 1988; 48(7):489–493. Doi: 10.1055/s-2008-1026525. (Originally published in German).
- Bordeianou L, Yeh DD. Epidemiology, Clinical Features, and Diagnosis of Mechanical Small Bowel Obstruction in Adults. UpToDate. https://www.uptodate.com/contents/epidemiology-clinical-features-and-diagnosis-of-mechanical-small-bowel-obstruction-in-adults. Accessed May 10, 2016.
- DynaMed, EBSCO Information Services. Pelvic vein thrombosis in women. DynaMed. https://www.ncbi.nlm.nih.gov/pubmed/11975950. Accessed May 11, 2017.
- Peiser BS. DynaMed, EBSCO Information Services. Venous Thromboembolism in pregnancy. DynaMed. 2016.
- Schwartz DR. Deep vein thrombosis in pregnancy: Epidemiology, pathogenesis, and diagnosis. UpToDate. https://www.uptodate.com/contents/deep-vein-thrombosis-in-pregnancy-epidemiology-pathogenesis-and-diagnosis. Accessed May 11, 2017.