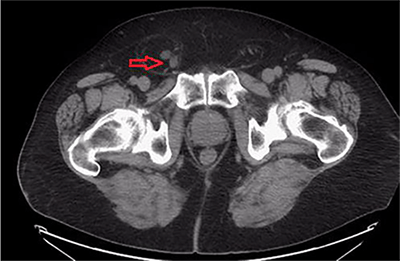
Figure 4. Coronal view of same study showingbilateral renal calculi with significant right sided hydronephrosis
Urology was consulted and a stent placement was attempted for decompression, but was unsuccessful given the tortuosity of the ureter. Subsequently, given the acute renal function impairment interventional radiology placed a 10 French percutaneous nephrostomy tube for decompression and to relieve the obstruction. At this time, the general surgery service was consulted for repair of the right inguinal hernia.
Operative Intervention
Under general anesthesia a standard right groin incision was made above the inguinal ligament. The external oblique aponeurosis was exposed and opened. Care was taken to protect the genital branch of the genitofemoral and ilioinguinal nerves. We encountered a large direct hernia, which was reduced from the scrotum. There was a large amount of fat present, but no bowel was seen. The ureter was not visualized and no attempt was made to explore the sac, thus protecting the viability of the structure. The sac was carefully dissected intact off of the cord structures up to the level of the internal ring and all the contents were reduced into the abdomen. The cord structures, including the venous plexus and vas deferens, were adequately identified and protected. A tension-free repair with mesh was performed to reconstruct the inguinal floor. The mesh was secured to the pubic tubercle and the inguinal ligament inferiorly and laterally. Superiorly, it was affixed to the conjoined tendon. The incision was closed in layers including: the external oblique aponeurosis, Scarpa's fascia and skin. The patient tolerated the procedure well. He recovered successfully in the standard time and fashion and was followed in clinic with both urology and surgery without any complications. Given his clinical improvement, normal laboratory values and urine output, the nephrostomy tube was removed on day 3 during the post-operative period.
Discussion
Involvement of the ureter in an inguinal hernia is uncommon given its retroperitoneal position with very few reported cases in the literature. This is particularly true in adult patients and with native kidneys. The prevalence of ureter-containing inguinal hernias is unclear but is very low. In 2012, one group quantified only 10 reports of this case.3 Another group analyzed 1,950 cases of operable inguinal hernias at their institution and did not identify any involvement of the ureter.
Contents present in inguinal hernias are varied, with fat and bowel being the most common. One study reported unusual herniated contents through the inguinal canal, which included: the vermiform appendix (0.51 percent), appendix with acute inflammation (0.10 percent), ovaries and fallopian tubes (2.9 percent), and the urinary bladder (0.36 percent).4
In regards to the ureter, a group described two anatomical variations of ureter-containing hernias in a case series. The paraperitoneal type (our patient), which represents about 80% of cases, where the ureter slides besides the peritoneal sac and frequently contains other organs such as the colon. The extraperitoneal form, 20 percent of cases, is characterized by the lack of a peritoneal sac with the ureter present within the retroperitoneal fat.5
The open surgical repair of an inguinal hernia follows a standard approach and its principles should be practiced in every case. In cases that present with unusual hernia sac contents, some precautions can be made preoperatively. One group presented a similar case to our report and described placing preoperative ureteral stents to aid with dissection and to protect the structure during hernia repair.6 Even though the role of preoperative ureteral stenting is not defined in this setting, surgeons might find them helpful for identification of this structure. The attempted stent placement on our patient was performed with the goal of decompression of the urinary system and to allow for resolution of the acute renal failure before the surgical consultation.
In this case we proceeded with an open approach due to surgeon’s comfort level in trying to maximize the protection of the ureter. One group recommended dissecting the ureter from the herniated contents to avoid iatrogenic injury;2,5,6 however, in this instance given the unsuccessful attempt of preoperative stenting, once we dissected the sac we were able to reduce the herniated contents back into the peritoneal cavity. We then proceeded with the reconstruction of the inguinal floor.
Minimally invasive techniques for inguinal hernia repair have been uniformly adopted by many practices for the repair of inguinal hernias. Such is the case of the recent report of one group, who described a successful robotic approach for the repair an extraperitoneal ureteral inguinal hernia.7 Although it can be accomplished successfully, surgeons must follow their level of comfort with such challenging cases.
Conclusion
Involvement of the ureter within an inguinal hernia is rare and can pose a surgical challenge. Based on the literature, our experience and available imaging suggesting ureteral compromise with obstruction or significant tortuosity, we recommend an open surgical approach with or without preoperative ureteral stent placement that can potentially assist in identification of the structure and protect its viability during dissection.
Lessons Learned
Early surgical consultation is warranted for a non-reducible hernia that can compromise viability to vital structures. CT or intravenous urologic studies are not necessary before every complex inguinal hernia operation.
Authors
Juan P. Gurria, MD
University of Illinois College of Medicine at Peoria. Division of General Surgery
Steven M. Henriques, MD
University of Illinois College of Medicine at Peoria. Division of General Surgery
Kimberly Helmkamp, MD
University of Illinois College of Medicine at Peoria. Division of Medicine-Pediatrics
Correspondence Author
Juan Gurria, MD
Division of Pediatric General and Thoracic Surgery
Trauma Surgery Fellow
Cincinnati Children's Hospital Medical Center
3333 Burnet Ave.
ML 2023
Cincinnati, OH 45229
713-291-6850
Juan.Gurria@cchmc.org
Disclosure Statement
The authors whose names are listed immediately above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Venara A, Hubner M, Le Naoures P, Hamel JF, Hamy A, Demartines N. Surgery for incarcerated hernia: short-term outcome with or without mesh. Langenbecks Arch Surg. 2014;399:571-7.
- Ballard JL, Dobbs RM, Malone JM. Ureteroinguinal hernia: a rare companion of sliding inguinal hernias. Am Surg. 1991;57:720-2.
- Won AC, Testa G. Chronic obstructive uropathy due to uretero-inguinal hernia: A case report. Int J Surg Case Rep. 2012;3:379-81.
- Gurer A, Ozdogan M, Ozlem N, Yildirim A, Kulacoglu H, Aydin R. Uncommon content in groin hernia sac. Hernia. 2006;10:152-5.
- Zmora O, Schachter PP. Sliding inguinal hernia containing the ureter: a case report. J Urol. 1996;155:1387.
- Latowsky J, Shenoy S. Ureteral inguinoscrotal hernia: a hidden hazard, stents may prevent injury. Am Surg. 2013;79:E133-4.
- Pucheril D, Chun B, Dalela D, Abdollah F, Laker SA, Rogers CG. Robot-Assisted Laparoscopic Repair of Extraperitoneal Ureteral Inguinal Hernia with Mesh Placement. J Endourol Case Rep. 2017;3:97-100.