Figure 6. Laparoscopic view of left colon on right with cecum and staple line of appendectomy in the middle
Discussion
After the fifth week of development, the gut is divided into three components: the foregut, the midgut, and the hindgut. Embryological abnormalities of the gastrointestinal tract can cause malrotation of the midgut.3 The midgut is the portion of the embryo from which the intestines develop. It begins from the end of the foregut at the beginning of the bile duct and continues to about two-thirds of the transverse colon. During development, the midgut grows rapidly and physiologically herniates outside of the abdominal cavity into the umbilical cord. After the midgut rotates around the superior mesenteric artery, it forms a midgut loop. Once the body of the fetus catches up with the midgut, the physiologically herniated portion moves out of the umbilical cord and therefore, ceases to exist. The arterial supply of the midgut is from the superior mesenteric artery, a branch of the aorta. The venous supply of the midgut is via the portal venous system and the lymph drainage is through the paravertebral superior mesenteric nodes.7
Intestinal rotation anomalies primarily involve the midgut. In stage 1 anomalies, the midgut fails to return from its physiologic herniation into the umbilical cord back into abdominal cavity.1 This leads to an omphalocele, in which the midgut protrudes from the abdominal cavity. In stage 2 anomalies, the midgut fails to rotate properly, doesn’t rotate at all, or rotates in a backward fashion. Stage 2 abnormalities lead to failure of the duodenum rotating behind the superior mesenteric artery as well as fluctuations in the proper positioning of the ascending colon, transverse colon and descending colon. Stage 3 of development includes the fusion and proper anchoring of the mesentery. Improper development of this stage can lead to a mobile cecum, an unattached duodenum or misaligned small bowel mesentery.9
Most acute presentations of intestinal malrotation are evident within the first month of life. Newborns typically present with abdominal pain and bilious vomiting. In adults with acute symptomatic intestinal malrotation, one of two common disease processes may develop. One group may develop symptoms of bowel obstruction with symptoms of abdominal pain, nausea, bilious vomiting, and constipation. Since the obstruction is most commonly proximally located, abdominal distension is not a common symptom. The second group may present with signs and symptoms of volvulus due to peritoneal bands constricting and compressing superior mesenteric vessels.6 This can cause the bowel to become infarcted and fill with blood, as venous drainage is blocked. These patients can present with intermittent constipation and mild abdominal pain. If the volvulus is relieved spontaneously, patients present with blood-tinged diarrhea due to the infarcted bowel bleeding into the lumen.
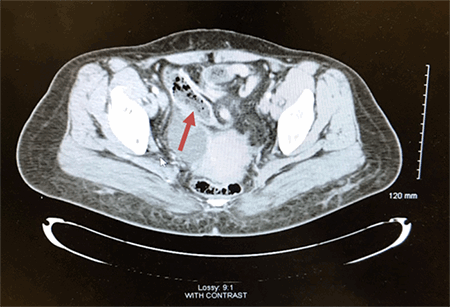
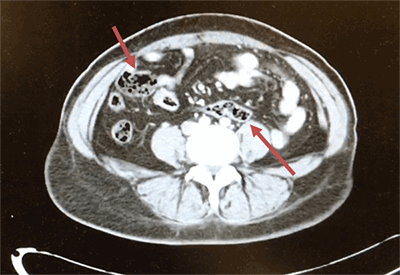
The diagnosis of intestinal malrotation is most commonly diagnosed with either upper GI tract contrast imaging or a barium enema. A CT scan can also be useful in identifying the abnormal locations of the intestine. The classical treatment for intestinal malrotation is the Ladd procedure.5 This procedure consists of mobilizing the duodenum and the right colon as well as the Ladd’s bands (periotoneal bands) and possible adhesions near the superior mesenteric vessels. An appendectomy is also commonly performed as diagnosing future conditions of would prove to be difficult since the appendix is not located in the classical lower right quadrant. The overall purpose of the Ladd procedure is to reduce the risks of intestinal ischemia and volvulus by locating the small intestine and widening the mesenteric base.
It is quite unusual to diagnose a patient with incidental intestinal malrotation and acute appendicitis due to the varying location of the appendix. Most patients experience vague abdominal pain that often cannot be ruled out via clinical diagnosis. Moreover, due to the abnormal location of the appendix and intestines, patients do not present with typical symptoms of acute appendicitis.2 The most important differential tools in such cases are imaging studies of the abdomen and pelvis. Early clinical suspicion and an adequate CT of the abdomen and pelvis are crucial in diagnosing acute appendicitis in a patient with possible intestinal malrotation. Failure to detect early appendicitis can lead to appendiceal perforation and possible abscess formation.
Conclusion
Intestinal malrotation in adults is rare and can be presented as either acute intestinal obstruction or chronic abdominal pain. The best surgical management is performing the Ladd procedure to prevent intestinal ischemia and volvulus.
Lessons Learned
Intestinal malrotation can lead to obstruction or volvulus. Early detection and treatment are critical to prevent intestinal ischemia. The Ladd procedure and an appendectomy are commonly performed in adults with intestinal malrotation.
Authors
Sheliza Kabani, MD
California Hospital Medical Center
Department of Surgery
Los Angeles, CA
Gudata S. Hinika, MD, FACS
California Hospital Medical Center
Department of Surgery
Los Angeles, CA
Correspondence Author
Sheliza Kabani, MD
California Hospital Medical Center
Department of Surgery
Los Angeles, CA 90015
310-954-7874
Sheliza.kabani@gmail.com
Disclosure Statement
The authors whose names are listed immediately above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Gohl ML, DeMeester TR. Midgut nonrotation in adults. An aggressive approach. Am J Surg 1975;129:319-23.
- Hou SK, Chern CH, How CK, Kao WF, Chen JD, Wang LM, et al. Diagnosis of appendicitis with left lower quadrant pain. J Chin Med Assoc. 2005;68:599–603.
- Hsu SD, Yu JC, Chou SJ, Hsieh HF, Chang TH, Liu YC. Midgut volvulus in an adult with congenital malrotation. Am J Surg 2008;195:705-7.
- Krapfer SA, Rappold JF. Intestinal malrotation—not just the pedriatric surgeon's problem. J Am Coll Surg 2004;199(4):628-35.
- Matzke GM, Dozois EJ, Larson DW, Moir CR. Surgical management of intestinal malrotation in adults: comparative results for open and laparoscopic Ladd procedures. Surg Endosc 2005; 19(10):1416-9.
- Pelucio M, Haywood Y. Midgut volvulus: an unusual case of adolescent abdominal pain. Am J Emerg Med 1994;12:167-71.
- Sadler TW, Langman J. Langman’s medical embryology. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. p. 60-110.
- Seymour NE, Andersen DK. Laparoscopic treatment of intestinal malrotation in adults. JSLS 2005;(9):298-301.
- Spigland N, Brandt ML, Yazbeck S. Malrotation presenting beyond the neonatal period. J Pediatr Surg 1990;(25):1139-42.