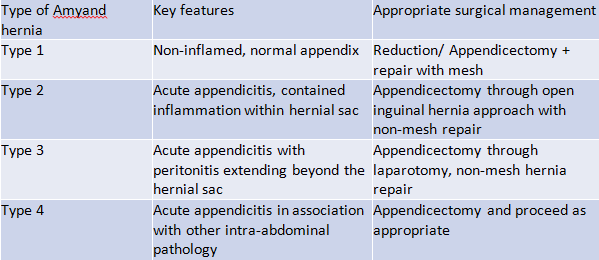
Table 1. Losanoff and Basson’s classification of Amyand hernia
An additional element to our case was the presence of a GCC within the appendix. GCCs are rare tumors of the appendix that often present with acute appendicitis, but can also present with vague abdominal pain/mass, rectal bleeding or intussusception.8 They are very aggressive, between 15 and 30 percent metastasis compared to two to five percent of typical appendiceal carcinoids.8 They often require further surgical management such as a right hemicolectomy with additional adjuvant therapy, and thus, a multidisciplinary approach is favored in this instance.8
Conclusion
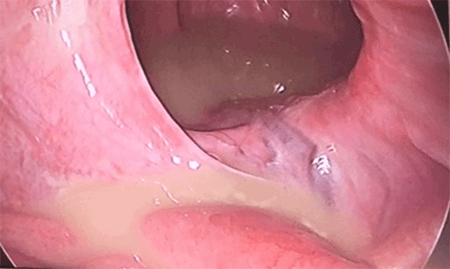
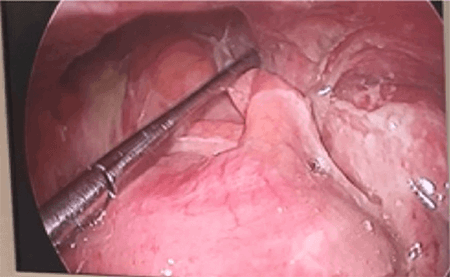
A presentation of perforated appendicitis with generalised peritonitis inside an Amyand hernia and managed laparoscopically is a rare occurrence, made rarer still by the presence of a GCC. While in this case, the diagnosis was suspected prior to arriving in theater, difficulty in preoperative diagnosis is well-documented, and any suspicion of complication (as was the case here) should warrant consideration of a diagnostic laparoscopy. In this case, the use of CT imaging was very helpful with diagnosis, and the laparoscopic approach was effective in achieving appendicectomy and source control for intra-abdominal sepsis.
Lessons Learned
A perforated appendix within an Amyand hernia is an exceptionally difficult preoperative diagnosis and often mimics an incarcerated inguinal hernia. Presentations of incarcerated inguinal hernia with atypical features should warrant consideration of this differential diagnosis. Traditionally, Amyand hernias have been managed with an open technique, but here, we demonstrate the advantages of a laparoscopic approach.
Authors
Williams M
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Ranasinghe S
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Wheatley L
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Anguswamy N
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Carrol J
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Walker D
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Lisec C
Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
Department of General Surgery, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia
Correspondence Author
Michael Williams
Department of General Surgery, Royal Brisbane and Women's Hospital Herston, Queensland, Australia
Phone: 0433165992
michael.williams6@health.qld.gov.au
Disclosure Statement
The authors whose names are listed immediately above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Fonesa-Neto O, Lucena R, Lacerda C. Amyand Hernia: inguinal hernia with acute appendicitis. Arq Bras Cir Dig. 2014 Nov-Dec;27(4):309-10.
- Morales-Cárdenas A, Ploneda-Valencia C, Sainz-Escárrega V et al. Amyand hernia: Case report and review of the literature. Ann Med Surg (Lond). 2015;4:113-115.
- Tsang W, Lee K, Tam K, Lee S. Acute appendicitis complicating Amyand hernia: imaging features and literature review. Hong Kong Med J. 2014;20:255-257.
- Feitosa Cavalcante J, Melo Teixeira Batista H, Cavalcante Pita Neto I et al. Amyand Hernia with Appendicitis: A Case Report and Integrative Review. Case Rep Surg. 2015;2015:941039.
- Ivashchuk G, Cesmebasi A, Sorenson E, Blaak C, Tubbs S, Loukas M. Amyand hernia: a review. Med Sci Monit. 2014 Jan 28;20:140-6.
- Kouskos E, Komaitis S, Kouskou M, Despotellis M, Sanidas G. Complicated acute appendicitis within a right inguinal hernia sac (Amyand hernia): report of a case. Hippokratia. 2014;18:74-76.
- Al-Ramli W, Khodear Y, Aremu M, El-Sayed A. A complicated case of Amyand hernia involving a perforated appendix and its management using minimally invasive laparoscopic surgery: A case report. Int J Surg Case Rep. 2016;29:215-218.
- Yahya Z, Wang C, Hong B. Amyand hernia containing an appendiceal goblet cell carcinoid tumor. BMJ Case Rep. 2017 Mar 16;2017.