We used a chevron incision for this operation. The right gastroepiploic artery was dissected out and a vessel loop was placed around it. The transverse colon at the level of hepatic flexure was mobilized, followed by dissection of duodenum from its retroperitoneal attachments. A Kocher maneuver was performed to expose the retroperitoneal structures. The fourth portion of the duodenum was then taken down with the ligament of Treitz, going above and below the transverse mesocolon. Because there was no previous Kocher maneuver or pyloroplasty, the dissection in this area was completed without significant inflammation or difficulty.
The mass was deemed resectable, and dissection was continued to the porta hepatis. The hepatic duct/common bile duct and GDA were visualized and dissected out. Vessel loops were placed around the GDA.
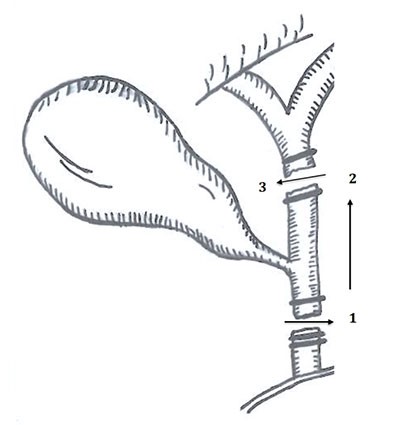
To preserve the gastric conduit flow for as long as possible, the GDA was not immediately transected. The specimen was dissected along the superior mesenteric vein, behind the pancreas, across the portal vein and above the superior edge of the pancreas. The pancreas was transected as was the duodenum just distal to the pylorus, ligating the right gastroepiploic at this time. The patient was then heparinized and an arteriotomy in the common hepatic artery was created. The mobilized right gastroepiploic artery was then transposed and anastomosed in an end to side fashion to the common hepatic artery, thereby preserving arterial inflow to the gastric conduit. Prior to reconstruction, patency was confirmed with Doppler evaluation, as well as completion angiogram via butterfly catheterization and contrast angiography on the table (Figure 1). We chose to anastomose the right gastroepiploic artery to the common hepatic artery instead of the GDA stump because the diameter of the common hepatic artery, tension on the anastomosis, and angulation of the anastomosis were superior. Intraoperative angiogram was performed which confirmed no thrombosis, flap, or dissection existed and to visually assess the flow through our anastomosis (Figure 1).
The pancreaticoduodenectomy procedure was completed with a hepaticojejunostomy, pancreaticojejunostomy, and antecolic gastrojejunosotomy. A Witzel jejunostomy tube was also placed, hemostasis was achieved, and the incision was closed. The patient tolerated the procedure well.
The patient’s postoperative course was uncomplicated. She suffered from no postoperative gastric emptying issues, anastomotic leaks, or vascular complications related to her operation.
Discussion
Tumors with vascular involvement during a pancreaticoduodenectomy procedure can significantly increase the technical difficulty of the operation, or preclude a patient from surgery all together and has been well described in multiple case series.1,3 However, successful arterial reconstruction, like the one described here, opens the door for pancreaticoduodenectomy in patients who might have other types variant anatomy; this includes, patients with previous partial gastrectomy, roux-en-y bypass, and/or celiac stenosis. With vascular reconstruction, up to 20 percent of patients once deemed inoperable now may have a chance for successful surgical resection.5
In a retrospective study published by Tseng et al, 110 patients underwent vascular reconstruction at the time of pancreaticoduodenectomy compared to 181 patients who underwent standard pancreaticoduodenectomy. The intervention group had a median survival of 23.4 months which did not significantly differ from the 26.5 month survival in the standard resection group. A key point, however, was that pancreaticoduodenectomy with vascular reconstruction was shown to be better than nonoperative management.6
These results are in concordance with a study by Gong et al, which found that the median survival time of the 119 cases that received vascular resection and reconstruction during pancreaticoduodenectomy was 13.3 months. The postoperative complication incidence was 23.5 percent, and the mortality was 6.7 percent; for the group without vascular reconstruction, complications occurred in 8.2 percent of cases and mortality was 3.0 percent. Thus, while there was a significant difference between the two groups in terms of complication rate, the difference in mortality rates was not significant. Like the conclusion drawn by Tseng et al, the median survival time was greater in patients who underwent pancreaticoduodenectomy with vascular reconstruction compared to those of patients who had no operative management at all, undergoing only palliative treatment for pancreatic cancer.7
Previous papers have reported operations in which arterial reconstruction was completed with splenic artery or GDA transposition4,8 or venous reconstruction of the SMV.1,5 However, extensive literature search has not yet identified a pancreaticoduodenectomy combined with vascular reconstruction due to altered anatomy from previous Ivor-Lewis esophagectomy. We were able to successfully reconstruct the blood supply to the patient’s gastric conduit, allowing for R0 resection of her pancreatic adenocarcinoma. With increased likelihood for R0 resection utilizing vascular reconstruction in pancreaticoduodenectomy, there is hope for increased survival benefit for patients who would otherwise be managed nonoperatively.5
Conclusion
Pancreaticoduodectomy can be successfully performed in patients status post Ivor-Lewis esophagogastrectomy by creating anastomosis between the common hepatic artery and the right gastroepiploic artery.
Lessons Learned
Patients with altered anatomy due to previous surgical history of esophagectomy with creation of a gastric conduit can still be candidates for pancreaticoduodenectomy. Despite ligation of the GDA in the resection of the duodenum, which would otherwise compromise the gastric conduit, right gastroepiploic blood flow can be sustained via transposition and anastomosis to the common hepatic artery.
Authors
Paige Finkelstein, BS
Department of General Surgery
University of Miami, Miller School of Medicine—JFK Regional Campus
Atlantis, FL
Kandace Kichler, MD
Department of General Surgery
University of Miami, Miller School of Medicine—JFK Regional Campus
Atlantis, FL
Joshua Parreco MD
Department of General Surgery
University of Miami, Miller School of Medicine—JFK Regional Campus
Atlantis, FL
Miguel Lopez-Viego, MD, FACS
Department of General Surgery
University of Miami, Miller School of Medicine—JFK Regional Campus
Atlantis, FL
Correspondence
Miguel Lopez Viego, MD, FACS
Division of Surgery
University of Miami, Miller School of Medicine
JFK Medical Center
5301 S Congress Avenue
Atlantis, Florida 33462
Phone: 561-779-9823
Fax: 561-736-4635
E-mail: lopezviegomd@yahoo.com
Disclosures
The authors have no conflicts of interest to disclose.
References
- Cheung TT, Poon RT, Chok KS, et al. Pancreaticoduodenectomy with vascular reconstruction for adenocarcinoma of the pancreas with borderline resectability. World J Gastroenterol. 2014 Dec 14;20(46):17448-55
- Sullivan AO. Whipple pancreaticoduodenectomy: A historical comment. Gd Rounds. 2007;7:1-2.
- Varadhachary GR, Tamm EP, Abbruzzese JL, et al. Borderline Resectable Pancreatic Cancer: Definitions, Management, and Role of Preoperative Therapy. Ann Surg Oncol. 2006 Aug;13(8):1035-46
- Perinel J, Nappo G, El Bechwaty M, et al. Locally advanced pancreatic duct adenocarcinoma: pancreatectomy with planned arterial resection based on axial arterial encasement. Langenbecks Arch Surg. 2016 Dec;401(8):1131-1142.
- Sgroi MD, Narayan RR, Lane JS. Vascular reconstruction plays an important role in the treatment of pancreatic adenocarcinoma. J Vasc Surg. 2015 Feb;61(2):475-80.
- Tseng JF, Raut CP, Lee JE, et al. Pancreaticoduodenectomy with vascular resection: margin status and survival duration. J Gastrointest Surg. 2004 Dec;8(8):935-49.
- Gong Y, Zhang L, He T, et al. Pancreaticoduodenectomy combined with vascular resection and reconstruction for patients with locally advanced pancreatic cancer: a multicenter, retrospective analysis. PLoS One. 2013 Aug 2;8(8):e70340.
- Fischer CP, Rosenberg W, Bridget F, Bass B. Gastroduodenal artery used for arterial reconstruction during the Whipple operation. Hepatogastroenterology. 2007 Dec;54(80):2228-9.