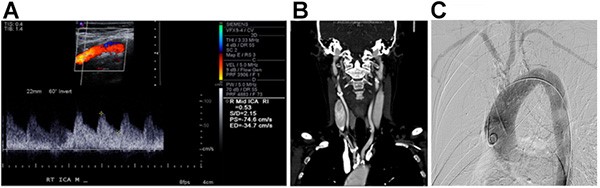
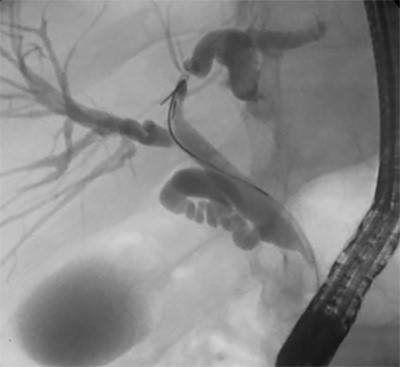
Despite percutaneous transluminal coronary angioplasty and bare metal stent placement, the patient’s LVEF consistently remained around 25 percent on repeat echocardiograms. His troponin level gradually trended down, however he demonstrated persistent ST elevation on telemetry suggestive of microvascular obstruction. In addition to dual antiplatelet therapy with aspirin and clopidogrel, he was prescribed a daily beta blocker and angiotensin converting enzyme inhibitor for mortality benefits secondary to his ischemic cardiomyopathy. Given the patient’s precarious cardiac status, orthopedic surgery postponed all operative interventions until a later date. The patient was eventually discharged to an acute rehabilitation facility. At the time of discharge, the patient was asymptomatic from a cardiac standpoint. Despite the absence of congestive heart failure symptoms, Follow-up myocardial perfusion imaging did not demonstrate thrombosis of the stent, yet surveillance echocardiograms demonstrated gradual decline in the patient’s LVEF despite pharmacologic optimization. An implantable cardioverter defibrillator was placed for primary preventative measures , however there are no plans for left ventricular assist device placement or cardiac transplantation unless the patient were to become symptomatic.
Discussion
It is presumed that extrinsic compression of the chest wall or sudden deceleration forces can produce a shearing of the coronary vessel wall, which then produces intimal tearing and subintimal hemorrhage. The tear activates platelet aggregation, fibrin, and other clotting cascade components precipitating intraluminal thrombus formation, with or without coronary spasm.10-12 The intraluminal thrombus, coronary spasm, or combination of the two can eventually lead to coronary artery occlusion. The LAD artery appears to be the most commonly affected vessel with involvement in 76 percent of cases. Comparatively, the right coronary artery is afflicted in 12 percent of cases, while the circumflex artery is afflicted in only six percent of cases.7,10 It is hypothesized that the anatomic location of the LAD artery, specifically the junction of the proximal and mid-portions, place it at greater risk of extrinsic compression from the anterior chest wall.10,11
The manifestations of traumatic coronary artery dissection are variable. Depending on the expansion of the false lumen, symptoms may not present for several days, or even weeks, following the inciting event.13,14 In certain situations, the dissection may be observed and treated conservatively, whereas in other cases it has the potential to generate malignant ventricular arrhythmias and could result in sudden cardiac death.15 As seen in this patient, coronary artery dissection can lead to coronary ischemia and myocardial infarction. Acute ECG changes in the setting of blunt chest trauma should trigger prompt cardiovascular evaluation, including serial cardiac enzymes and echocardiography.15 In the setting of coronary artery dissection, early recognition and diagnosis with transesophageal echocardiogram or coronary angiography may limit the impact of the infarction.10,16,17 For this particular patient, there are several possibilities as to why the myocardium did not regain function. One potential explanation could be the presence of direct myocardial contusion. While the presence of direct myocardial contusion could have conceivably exacerbated the myocardial ischemia caused by the coronary artery dissection, it ultimately would not have changed patient’s treatment strategy. An additional possibility may have been persistent microvascular occlusion and lack of microvascular integrity. Alternatively, a study by Ito et al suggested that abrupt restoration of myocardial blood flow by angioplasty could worsen the damage of the post-ischemic coronary microvasculature.18
Due to its rare occurrence, the optimal treatment of traumatic coronary artery dissection is currently not well-established, therefore management must be individualized.6,8,16 Based on how a patient presents, one may pursue conservative management, angiography with stenting, surgical revascularization, or thombolytic therapy.11 In the presence of occlusion or stenosis, reperfusion may be achieved by means of direct angioplasty.17 The use of thrombolytics in polytrauma patients remains controversial.16,17 Furthermore, there is concern that thrombolytic therapy could worsen dissections in the acute phase.8 Although the patient’s myocardium ultimately did not regain function following angioplasty and stenting, it is difficult to know whether an alternative management strategy would have been more advantageous, Surgical revascularization in the form of coronary artery bypass is a maximally invasive procedure compared to cardiac catheterization, and the associated morbidity and mortality risks did not outweigh the potential benefits in this particular patient at initial presentation. For these reasons, we would likely implement the same management strategy for similar cases in the future. Had there been evidence of stent thrombosis on repeat myocardial perfusion imaging, the option of surgical revascularization would have been reconsidered.
There are a variety of factors that can affect a patient’s prognosis, with severity and duration of vessel occlusion being of particular importance.8 It is thought that in the absence of ongoing ischemia, complete healing of traumatic coronary occlusion occurs within six months of initial injury. However, these patients are still at risk of developing aneurysmal disease.10 In addition, there are concerns that a persistent intimal flap could act as a nidus for rethrombosis, ultimately leading to restenosis.12 In regards to prognosis, our patient’s three year mortality risk is less than ten percent based on the Meta-Analysis Global Group in Chronic Heart Failure Risk Calculator, This case illustrates the complexities of the decision-making process involved with caring for polytrauma patients. Although the patient suffered permanent cardiac damage related to his traumatic injuries, he was still been able to achieve an acceptable quality of life in the post-recovery period.
Conclusion
Albeit rare, coronary artery dissections are a potentially life-threatening complication of blunt chest trauma. This report describes the case of a healthy young male presenting after a motor vehicle collision, and subsequently found to have a proximal dissection of the left anterior descending artery leading to an anterior wall myocardial infarction. It highlights the importance of prompt cardiovascular workup initiation by trauma surgeons for patients complaining of chest pain after having sustained blunt chest trauma.
Lessons Learned
The manifestations of traumatic cardiac injury may present hours, days, or weeks after the inciting event. The management of traumatic coronary artery dissection remains disputed due to its rare occurrence. Patient prognosis is variable and dependent on the extent of vessel occlusion.
Abbreviations
LVEF: left ventricular ejection fraction
LAD: left anterior descending
ECG: electrocardiogram
Authors
Jessica L. Thompson, MD
Grand Rapids Medical Education Partners
Division of General Surgery
Grand Rapids, MI
Cathryn L. Chadwick
Spectrum Health
Division of Acute Care Surgery
Grand Rapids, MI
Correspondence
Dr. Jessica Thompson
2370 Farm Court SE
Grand Rapids, MI 49546
Phone: 906-322-0950
E-mail: 1thompsonjessica@gmail.com
Disclosures
The authors have no conflicts of interest to disclose.
References
- Coimbra R, Hoyt DB. Chest wall trauma, hemothorax, and pneumothorax. In Cameron JL, Cameron AM, eds. Current Surgical Therapy. 11th ed. Philadelphia, PA: Elsevier Saunders; 2014:1005-1009.
- Schaider J, Barkin RM, Rosen P. Rosen & Barkin's 5-minute emergency medicine consult. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- Prêtre R, Chilcott M. Blunt trauma to the heart and great vessels. N Engl J Med. 1997;336(9):626-32.
- Fousas SG, Athanasopoulos GD, Cokkinos DV. Myocardial infarction caused by blunt chest injury: possible mechanisms involved: case reports. Angiology. 1989 Apr;40(4 Pt 1):313-318.
- Vlay SC, Blumenthal DS, Shoback D, et al. Delayed acute myocardial infarction after blunt chest trauma in a young woman. Am Heart J. 1980;100:907-16.
- Swinkels BM, Hoedemaker G, Peters RHJ. Coronary artery dissection following blunt chest trauma: a case report. Neth Heart J. 2005;13(5):190-92.
- Mubang RN, Hillman Terzian WT, Cipolla J, et al. Acute myocardial infarction following right coronary artery dissection due to blunt trauma. Heart Views. 2016;17(1):35-38.
- Chun JH, Lee SC, Gwon HC, et al. Left main coronary artery dissection after blunt chest trauma presented as acute anterior myocardial infarction: assessment by intravascular ultrasound: a case report. J Korean Med Sci. 1998;13:325-27.
- Liedthe J, DeMuth W. Nonpenetrating cardiac injuries: a collective review. Am Heart J. 1973;86:687-97.
- Yang S, Zhou Y, Guo Z, et al. The natural course of traumatic myocardial infarction in a young patient with angiographically normal coronary arteries. Heart Lung. 2012;41(3):294-300.
- Hobelmann A, Pham JC, Hsu EB. Right coronary artery dissection following sports-related blunt trauma. Emerg Med J. 2006;23:580-81.
- Kohli S, Saperia GM, Waksmonski CA, et al. Coronary artery dissection secondary to blunt chest trauma. Cathet Cardiovasc Diag. 1998;15:179-83
- Rubin DA, Denys BG. Delayed and spontaneous coronary artery rupture following nonpenetrating chest trauma. Am Heart J. 1992;124:1635-37.
- Guldner GT, Schilling TD. Coronary artery occlusion following blunt chest trauma: a case report and review of the literature. CJEM. 2005;7(2):118-23.
- Van Mieghem NM, van Weenen S, Nollen G, et al. Traumatic Coronary Artery Dissection. Potential Cause of Sudden Death in Soccer. Circulation. 2013;127:e 280-82.
- Ginzburg E, Dygert J, Parra-Davila E, et al. Coronary artery stenting for occlusive dissection after blunt chest trauma. J Trauma. 1998;45(1):157-61.
- Adler JD, Scalea TM. Right coronary artery dissection after blunt chest trauma. Injury. 2010;41(8):77-79.
- Ito H, Tomooka T, Sakai N, et al. Lack of myocardial perfusion immediately after successful thrombolysis a predictor of poor recovery of left ventricular function in anterior myocardial infarction. Circulation. 1992;85:1699-1705.