Abstract
Background
Colonic lipomas are a rare entity and are reported in the literature with a variety of presentations. Although they can mimic malignant lesions, they are benign proliferative lesions of fatty tissue arising from the submucosa of the intestine. They can present with crampy abdominal pain associated with obstruction, and they most commonly present with intussusception and bowel obstruction. They are also reported as causes of gastrointestinal bleeding. Microscopic submucosal lipomas with mucosal ulceration associated with either chronic anemia and slow gastrointestinal bleeding or intermittent bleeding causing bright red blood per rectum have not been reported in the literature.
Summary
We report a case in which microscopic submucosal lipomas were associated with bright red blood per rectum with an initial presentation of sepsis secondary to colitis. A 55-year-old female admitted with the diagnosis of colitis started having a drop in hemoglobin and bloody bowel movements. A CTA and nuclear scan could not locate the source of bleeding. She had findings of sigmoid and transverse colon colitis on CT scan. Colonoscopy showed sigmoid and ascending colon colitis without any evidence of active bleeding. The patient was taken to the operating room in the setting of bleeding refractory to conservative management, and a right colectomy was performed. The specimen showed scattered ulceration of the ascending colon and a friable terminal ileum.
Conclusion
The patient’s hemoglobin was stable after the surgery, and pathology showed submucosal lipomatosis with overlying mucosal ulcerations. Microscopic submucosal lipomatosis with mucosal ulceration may present as intermittent bleeding. Pathologists should keep this differential in mind because it may lead to differences in management.
Key Words
Colonic lipomas, colonic lipomatosis, submucosal colon lipoma, colon mucosal ulceration, submucosal lipomatosis, bowel lipoma
Colonic lipomas are a rare entity and are reported in the literature with a variety of presentations. In the myriad of a long list of differential diagnoses for bright red blood per rectum, colonic lipomas should have their own place. Although colonic lipomas can mimic malignant lesions, they are benign proliferative lesions of fatty tissue arising from the submucosa of the intestine. Lipomatous disease of the intestine is a rare phenomenon that mostly presents in the colon with right-sided predominance. It is a disease of the older age group, with predominance in the sixth decade of life. Most of the time, these are asymptomatic lesions found incidentally on endoscopy or on CT scan done for other reasons.1 The lesions have been reported as incidental findings upon autopsy, with an incidence of 0.3-0.5 percent.2 The fatty proliferation leads to an appearance of pedunculated polyps, and, when multiple in number, can be hard to differentiate from familial adenomatous polyposis.3 The intraluminal growth and polyp formation mostly causes crampy abdominal pain associated with obstruction, and the condition most commonly presents with intussusception and bowel obstruction.4 This entity that is described in the literature with visible polyposis lipomatosis on colonoscopy is the most common presentation and is most commonly diagnosed on colonoscopy.
There are cases reported in the literature where colonic lipomas cause sigmoid perforation, mechanical obstruction of the transverse colon, and massive intestinal bleeding associated with hematochezia.5-7 A very small proportion of these colonic lipomas are associated with gastrointestinal bleeding. When the lipomas are small, biopsies of these lesions can miss the diagnosis if the pathologist is not looking for submucosal lipomas as part of the differential diagnosis. The lesions may simply be reported as colitis—this is what occurred in our case report.
The microscopic submucosal lipomas associated with mucosal ulceration (with either chronic anemia and slow gastrointestinal bleeding or with intermittent bleeding causing bright red blood per rectum) have not been reported in the literature. Our case involves microscopic submucosal lipomas associated with bright red blood per rectum with an initial presentation of sepsis secondary to colitis.
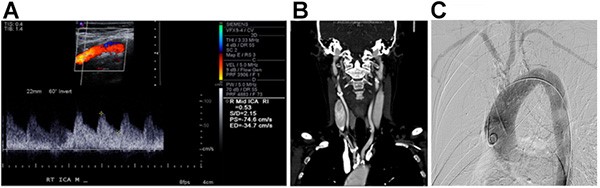
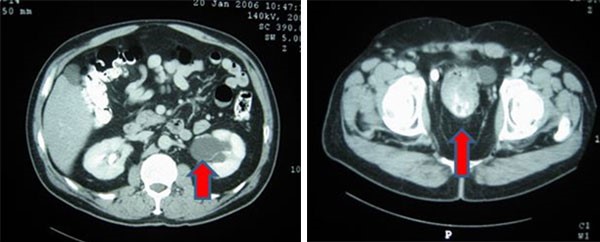
A 55-year-old female presented to the emergency room with bilateral lower abdominal crampy pain associated with two to three episodes of vomiting per day, six to seven episodes of non-bloody diarrhea, and subjective chills for the past four days. She denied any weight loss or any similar episodes in the past. Her last colonoscopy was performed four months prior and showed benign polyps. The patient denied a history of atrial fibrillation and was not on blood thinners. She had a past medical history of hypertension, hyperlipidemia, and chronic kidney disease stage 3. The patient also had a past surgical history of a left donor nephrectomy 10 years ago and laparoscopic cholecystectomy six years ago. She smoked half a pack of cigarettes per day for 25 years. The patient’s mother had end-stage renal disease, with no family history significant for inflammatory bowel disease or colon cancer. On physical exam of her abdomen, the patient had tenderness in the bilateral lower quadrants but no guarding. The patient had a temperature of 39.5°C in the emergency room, a heart rate of 120, and blood pressure= 90/56. Her white blood cell count was 3.0 and hemoglobin was 15.3, with a creatinine of 1.46 and lactic acid of 1.1. A CT scan was obtained, which showed mild sigmoid colitis and proximal to mid transverse colon colitis (Figures 1 and 2). Blood cultures were drawn, and the patient was started on broad spectrum antibiotics and was admitted.