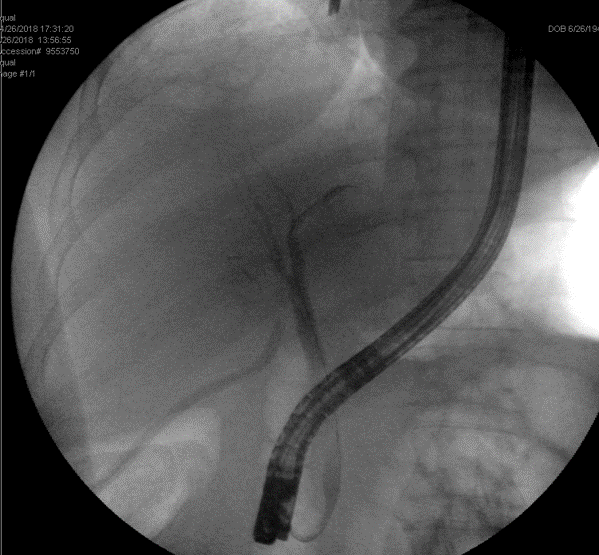
Figure 4A (Left). Patent jump graft (white arrow) to the portal vein on posttransplant day 7. Figure 4B (Right). Patent jump graft (white arrow) to the superior mesenteric vein one year postransplant.
Discussion
This is the first reported case to successfully utilize double prosthetic grafts for managing extensive PVT and for hepatic venous outflow reconstruction in LDLT.
Rapid restoration of portomesenteric inflow and venous outflow in the liver graft is critical in liver transplant. The safety and efficacy of using ePTFE grafts in the hepatic outflow reconstruction have been well established, with a low rate of stenosis, thrombosis, or infection. It can also reduce warm ischemic time by rapidly anastomosing a well-prepared customary prosthetic venous conduit to inferior vena cava.4 In our series, the two-month patency rate of ePTFE vascular graft was 100 percent, which is essential to substantial liver regeneration at the immediate posttransplant stage.4 However, prosthetic vascular grafts have never been reported with regards to reconstructing portomesenteric venous inflow in LDLT for patients with extensive PVT.
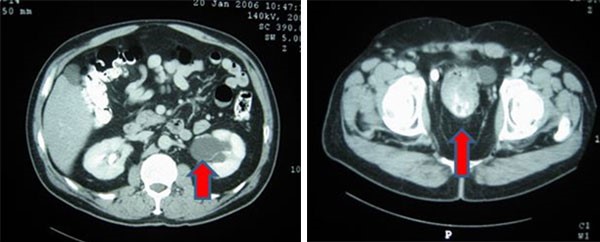
PVT secondary to underlying liver cirrhosis often makes surgery more challenging and increases operative complexity. Lower dissection of the portal vein and thrombectomy could resolve most of grade 1 or 2 PVT in liver transplant.2 However, an interposition or jump vascular graft may be needed in case of grade 3 or 4 PVT. Cryopreserved vascular graft is preferred as a jump graft for portomesenteric venous thrombosis because it is less thrombogenic and particularly helpful in a low-flow vascular system.1 That said, we still had to use non-ringed ePTFE prosthetic vascular grafts because of the unavailability of cryopreserved vascular graft in our hospital. To reduce ePTFE graft-related thrombogenic influence on the low-flow vascular system, we ligated all collateral varices around the superior mesenteric vein anastomosis site to increase portomesenteric flow. We believe that this maneuver is essential to increasing portovenous flow to the liver graft, particularly for those with extensive portomesenteric venous thrombosis accompanied by abundant collateral circulation.
After vascular reconstruction, antiplatelet and anticoagulant therapy were offered to the patient since posttransplant day three to reduce thrombogenic influence. Currently, antiplatelet rather than anticoagulant was suggested in patients who received ePTFE vascular graft for hepatic venous outflow reconstruction in LDLT.5 We prescribe 100mg of aspirin once a day for two years for those receiving prosthetic vascular grafts in hepatic venous outflow reconstruction.4 To ensure adequate portomesenteric venous inflow, the patient was provided antiplatelet and anticoagulant therapy concurrently while posttransplant hemorrhage was excluded.
Conclusion
Concurrently applying the ePTFE grafts for the inflow and outflow reconstruction may be a reliable alternative method in managing LDLT recipients with extensive PVT.
Lesson Learned
The patient was discharged on posttransplant day 20 without any sequelae and has been followed for one year without recurrent PVT. With our successful experience, we believe that ePTFE grafts used for the inflow and outflow reconstruction may be a reliable alternative method in managing LDLT recipients with extensive PVT.
Authors
Lorena Noriega-Salas, MDa,b; Chun Chieh Yeh, MDa,b,c; Horng-Ren Yang, MDa,b,c; and Long-Bin Jeng, MDa,b,c
Correspondence Author
Dr. Chun Chieh Yeh*
Organ Transplantation Center
China Medical University Hospital
2 Yuh-Der Road
Taichung, Taiwan, 40447
Phone: 04-22052121 Ext.1765
FAX: 04-22029083
transplantyeh@gmail.com
Author Affiliations
a Organ Transplantation Center, China Medical University Hospital, Taichung, Taiwan, 40447
b Department of Surgery, China Medical University Hospital, Taichung, Taiwan, 40447
c China Medical University, Taichung, Taiwan, 40447
Disclosure Statement
The authors have no conflicts of interest to disclose.
*Chun Chieh Yeh and Long-Bin Jeng contributed equally as co-corresponding authors
References
- Hwang HP, Yang JD, Bae SI, Hwang SE, Cho BH, Yu HC. Usefulness of artificial jump graft to portal vein thrombosis in deceased donor liver transplantation. Yonsei Med J. 2015;56(2):586-590.
- Kim SJ, Kim DG, Park JH, et al. Clinical analysis of living donor liver transplantation in patients with portal vein thrombosis. Clin Transplant. 2011;25(1):111-118.
- Sugawara Y, Makuuchi M, Tamura S, et al. Portal vein reconstruction in adult living donor liver transplantation using cryopreserved vein grafts. Liver Transpl. 2006;12(8):1233-1236.
- Thorat A, Jeng LB, Yang HR, et al. Outflow reconstruction for right liver allograft with multiple hepatic veins: "V-plasty" of hepatic veins to form a common outflow channel versus 2 or more hepatic vein-to-inferior vena cava anastomoses in limited retrohepatic space. Liver Transpl. 2016;22(2):192-200.
- Hwang S, Jung DH, Ha TY, et al. Usability of ringed polytetrafluoroethylene grafts for middle hepatic vein reconstruction during living donor liver transplantation. Liver Transpl. 2012;18(8):955-965.