
Percutaneous Cyanoacrylate Glue Injection: A Cost-Effective and Nonoperative Intervention for Persistent J Pouch Fistul
April 24, 2020
Abstract
Background
A 38-year-old male patient with a history of familial adenomatous polyposis (FAP) and carcinoma of the sigmoid colon underwent restorative proctocolectomy with an ileoanal anastomosis (J pouch) procedure. The patient later presented with an ileal pouch-anal anastomotic leak that presented as a pouch-cutaneous fistula to the anterior abdominal wall.
Summary
Our patient was managed conservatively with percutaneous drainage of intraabdominal collection and optimal nutritional management. There was no stenosis of the anastomosis. As the fistula failed to close after six months of conservative management, percutaneous injection of cyanoacrylate glue was done into the fistulous tract in order to avoid re-exploration. The tract closed, and the diverting ileostomy was closed after five months. There was no recurrence.
Conclusion
Percutaneous cyanoacrylate glue injection can be attempted for simple fistulae resulting from anastomotic leaks following restorative proctocolectomy.
Key Words
Familial adenomatous polyposis; FAP; J Pouch; Pouch fistula; Cyanoacrylate glue
Case Description
Ileal-pouch anal anastomosis (IPAA) is the treatment of choice for patients with familial adenomatous polyposis (FAP) and can be performed with low operative mortality, acceptable morbidity, and good functional outcomes.1 Anastomotic leaks occur in 6.5 to 7.3 percent of patients following IPAA. This may result in pouch- cutaneous fistulae2,3 causing major morbidity and pouch failure (22 to 35 percent).4 Failure of spontaneous closure may necessitate pouch revision, re-anastomosis, or pouch excision. Reoperation is associated with high morbidity and poor success rates. A nonoperative approach that limits the collateral damage is therefore desirable. We present a case of FAP. The patient had an anastomotic leak and pouch- cutaneous fistula following IPAA and was successfully managed with cyanoacrylate glue injection of the fistulous tract followed by closure of the diverting ileostomy.
A 38-year-old male presented with a history of FAP as well as three months of rectal bleeding. Colonoscopy was consistent with FAP and a moderately differentiated adenocarcinoma arising in a tubulovillous adenoma in the left colon. Metastatic workup was negative. After preoperative counselling and informed consent, the patient underwent a restorative proctocolectomy with IPAA using a standard double-stapled technique with a J pouch and diverting loop ileostomy. Patient was discharged on the 10th postoperative day. He was readmitted on the 20th postoperative day with fever, vomiting, abdominal pain, and low urine output. Laboratory workup revealed leucocytosis, deranged renal parameters, and metabolic acidosis. The patient was started on broad-spectrum antibiotics (imipenem and metronidazole), and his fluid and electrolyte balances were optimized. A CT of the abdomen showed a 9.2 x 3.9 cm collection in the left paracolic gutter with small air bubbles. Percutaneous drainage of collection was done with a 12 Fr catheter. The patient became afebrile with normalization of white cell counts and renal parameters. The percutaneous catheter was removed, and the patient was discharged after a two-week hospital stay; however, he was readmitted a month later with an abscess over the percutaneous drainage site. A CT scan with rectal water-soluble contrast showed extravasation of contrast in a long linear tract from the J pouch into the left paracolic gutter collection, which was contiguous with the abscess. An incision and drainage of the abscess was done, and a 10 Fr percutaneous catheter was inserted to drain the collection. Rectal examination and proctoscopy revealed an intact anastomotic ring with no stricture. However, the fistula failed to close after six months of conservative management. As the patient wished to avoid a reoperation, a nonoperative approach with percutaneous cyanoacrylate glue injection was attempted. A water-soluble contrast study through the infant feeding tube showed a long linear tract with opacification of the pouch (Figure 1).
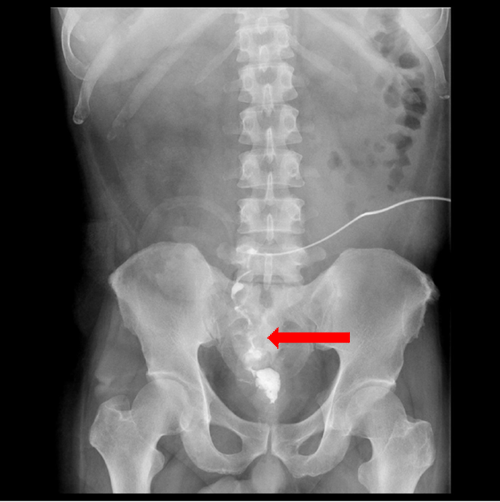
Figure 1. Contrast through catheter opacifying the tract and J Pouch
The internal opening was visualized with a flexible sigmoidoscope placed in the pouch. A new 10Fr infant feeding tube was inserted into the tract as far as it would go. A total of 2 mL of n- butyl-2-cyanoacrylate was injected rapidly through the tube until it was seen at the internal opening. The tube was then rapidly withdrawn while the injection was completed before the glue solidified. The patient was followed-up for five months and did not show recurrence of the fistula. A rectal contrast study did not demonstrate the fistula (Figure 2).

Figure 2. Rectal Contrast study showing obliteration of fistulous tract.
The patient demonstrated continence following rectal contrast. The ileostomy was closed two weeks later. The patient is currently on follow-up; his stool frequency is 8 to 10 times per day, he is continent, and there is no recurrence of the fistula.
Discussion
Hindgut fistulae have been treated by several nonoperative techniques; these include endoscopic and percutaneous techniques using metal clips,5 gel foam,6 fibrin glue,7 and cyanoacrylate glue.8 Gel foam and fibrin glue lack the tensile and adhesive strength that cyanoacrylates provide. Fibrin glue, being an animal protein, may be associated with problems of allergy and prion disease transmission. The compound may also be broken down by enzyme-rich fluid secreted in the gastrointestinal tract.9 Cyanoacrylates are a class of synthetic glues applied as monomers, which polymerize in an exothermic reaction when in contact with a weak base such as water and blood.10 They solidify within the tract and induce an inflammatory response that enhances fibrosis and foreign body granuloma formation with ultimate epithelization.11 They are also significantly cheaper than the other agents. A potential complication of glue is the possibility of gluing a delivery catheter into the tract. This can be avoided by stopping the injection and withdrawing the catheter when the glue approaches the catheter tip. The use of hydrophilic catheters has reduced the risk of adhesion.12 Cyanoacrylate glue may be mixed with lipiodol, an oily contrast agent, before injection; this slows the rate of solidification, thereby reducing the risk of inadvertent adherence to catheters endoscopes. It also allows for visualization of the injected glue. Various ratios of glue and lipiodol are used, ranging from 1:1 to 1:1.6.10 In the present case, hydrophilic catheters or lipiodol were not used due to severe financial constraints, but it may be desirable to use them to ease administration. In a study of percutaneous injection of fistulous tracts with cyanoacrylate and lipiodol, six patients with a total of seven postoperative low-output enterocutaneous fistulas (ECF) of the large intestine were treated. Complete closure of all seven fistulas was achieved.13 In another series where endoscopic injection was done in seven ECFs, closure was achieved in all cases. However, 30 percent patients required two or more sittings.8 Two cases of pouch fistulae were treated with an endoscopic injection of the tract under fluoroscopic guidance using fibrin glue. Both were successful with no recurrence of the fistula after 12 months.14 The present case is the first reported closure of a pouch fistula using cyanoacrylate injection through a percutaneous route.
Conclusion
The present case demonstrates that cyanoacrylate glue can be used effectively as a low-cost and nonoperative method of achieving closure of simple fistulae following pouch leaks. Its utility in more complex fistula remains to be determined.
Lessons Learned
Redo surgery for pouch failure is a daunting task and is associated with poor outcomes. Nonoperative techniques like cyanoacrylate glue injection may help in salvaging patients with pouch fistulae.
Authors
Jacob Mathew, MBBS, MS, MCh
Department of Surgical Gastroenterology and Liver Transplantation, VPS Lakeshore Hospital, Nettoor, Maradu PO, Kochi 682040, Kerala, India
Mahesh Subramanya Iyer, MBBS, MS, DNB
Department of Surgical Gastroenterology and Liver Transplantation, VPS Lakeshore Hospital, Nettoor, Maradu PO, Kochi 682040, Kerala, India
Roy Mukkada, MBBS, MD, DNB
Department of Medical Gastroenterology, VPS Lakeshore Hospital, Nettoor, Maradu PO, Kochi 682040, Kerala, India
Hariharan Ramesh, MBBS, MS, MCh, FACS, FRCS
Department of Surgical Gastroenterology and Liver Transplantation, VPS Lakeshore Hospital, Nettoor, Maradu PO, Kochi 682040, Kerala, India
Correspondence
Dr. Jacob Mathew
Department of Surgical Gastroenterology and Liver Transplantation
VPS Lakeshore Hospital
Nettoor
Maradu PO
Kochi 682040
Kerala, India
Email :drjacobmathew@gmail.com
Phone : +919526971696
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Fazio VW, Kiran RP, Remzi FH, et al. Ileal Pouch Anal Anastomosis Analysis of Outcome and Quality of Life in 3707 Patients Victor Warren. Ann Surg. 2013;257(4):679-685. doi:10.1097/SLA.0b013e31827d99a2.
- Lovegrove RE, Heriot AG, Constantinides V, et al. Meta-analysis of short-term and long-term outcomes of J, W and S ileal reservoirs for restorative proctocolectomy. Color Dis. 2007;9(4):310-320. doi:10.1111/j.1463-1318.2006.01093.x.
- Michelassi F, Lee J, Rubin M, et al. Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg. 2003;238(3):433-41-5. doi:10.1097/01.sla.0000086658.60555.ea.
- Johnson PM, O'Connor BI, Cohen Z, McLeod RS. Pouch-Vaginal Fistula After Ileal Pouch-Anal Anastomosis: Treatment and Outcomes. Dis Colon Rectum. 2005;48(6):1249-1253. doi:10.1007/s10350-004-0872-9.
- Kumar R, Naik S, Tiwari N, Sharma S, Varsheney S, Pruthi HS. Endoscopic Closure of Fecal Colo-cutaneous Fistula by Using Metal Clips. Surg Laparosc Endosc Percutan Tech. 2007;17(5):447-451. doi:10.1097/SLE.0b013e3180dc9392.
- Lisle DA, Hunter JC, Pollard CW, Borrowdale RC. Percutaneous Gelfoam Embolization of Chronic Enterocutaneous Fistulas: Report of Three Cases. Dis Colon Rectum. 2007;50(2):251-256. doi:10.1007/s10350-006-0772-2.
- Hwang T-L, Chen M-F. Randomized trial of fibrin tissue glue for low output enterocutaneous fistula. Br J Surg. 1996;83(1):112-112. doi:10.1002/bjs.1800830135.
- Billi P, Alberani A, Baroncini D, et al. Management of Gastrointestinal Fistulas with N-2-Butyl-Cyanoacrylate. Endoscopy. 1998;30(6):S 69-S 69. doi:10.1055/s-2007-1001352.
- Bège T, Emungania O, Vitton V, et al. An endoscopic strategy for management of anastomotic complications from bariatric surgery: a prospective study. Gastrointest Endosc. 2011;73(2):238-244. doi:10.1016/J.GIE.2010.10.010.
- Seewald S, Sriram PVJ, Naga M, et al. Cyanoacrylate glue in gastric variceal bleeding. Endoscopy. 2002;34(11):926-932. doi:10.1055/s-2002-35312.
- Willetts IE, Dudley NE, Tam PKH. Endoscopic treatment of recurrent tracheo-oesophageal fistulae: long-term results. Pediatr Surg Int. 1998;13(4):256-258. doi:10.1007/s003830050310.
- Mathis JM, Evans AJ, Denardo AJ, et al. Hydrophilic Coatings Diminish Adhesion of Glue to Catheter: An In Vitro Simulation of NBCA Embolization. AJNR Am J Neuroradiol. 1997;18:1087-1091. http://www.ajnr.org/content/ajnr/18/6/1087.full.pdf. Accessed December 12, 2017.
- Sapunar LC, Sekovski B, Matic D, Tripkovic A, Grandic L, Družijanic N. Percutaneous embolization of persistent low-output enterocutaneous fistulas. Eur Radiol. 2012;22(9):1991-1997. doi:10.1007/s00330-012-2461-y.
- Lamont JP, Hooker G, Espenschied JR, Lichliter WE, Franko E. Closure of proximal colorectal fistulas using fibrin sealant. Am Surg. 2002;68(7):615-618. http://www.ncbi.nlm.nih.gov/pubmed/12132744. Accessed December 13, 2017.