Large Bowel Obstruction Leading to Disseminated Salmonellosis: A Case Report and Review of the Literature
April 24, 2020
Abstract
Background
A 72-year-old male with a history of a deceased donor kidney transplant on prednisone and tacrolimus presented with a large bowel obstruction and subsequent disseminated salmonella infection.
Summary
The patient presented with several days of diarrhea that progressed to abdominal pain, nausea, and obstipation. CT scan revealed a large bowel obstruction, and the patient was taken to the operating room (OR) for enterolysis, which relieved the obstruction. On postoperative day five, the patient developed mixed hypercarbic-hypoxic respiratory failure secondary to salmonella pneumonia (serogroup BL L). He also developed hyperbilirubinemia without other liver function abnormalities consistent with salmonella hepatitis. Both the pneumonia and the hepatitis resolved with directed antimicrobial treatment.
Conclusion
In this case, a large bowel obstruction led to bacterial translocation of salmonella and subsequent disseminated infection manifest by hepatitis and pneumonia. Clinicians should be aware of potential risks of bacterial translocation in immunocompromised patients with bowel obstructions.
Key Words
large bowel obstruction, salmonella, salmonella hepatitis, salmonella pneumonia
Case Description
This report is of a 72-year-old male with a past medical history of renal failure, status post-deceased donor kidney transplant in 2013, hypertension, type 2 diabetes, hypercholesterolemia, coronary artery disease, and peripheral artery disease. The patient’s outpatient medications included tacrolimus, prednisone, carvedilol, clonidine, eplerenone, furosemide, hydralazine, injectable insulin, isosorbide mononitrate, losartan, methenamine, mycophenolic acid, nifedipine, omeprazole, simvastatin, and terazosin.
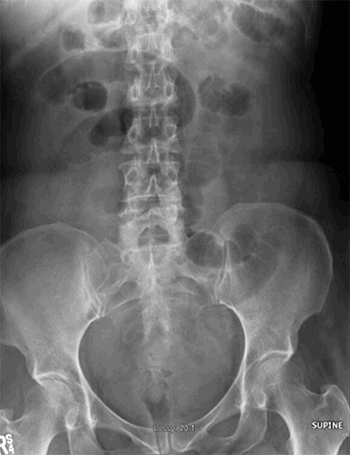
The patient initially presented to his outpatient nephrologist with three days of diarrhea without fever or pain. He had no known sick contacts, but had traveled to the Dominican Republic two weeks prior. Over the next by three days, the patient developed abdominal pain, nausea, vomiting, distention, and obstipation. He was sent to the emergency department (ED) by his nephrologist. In the ED, the patient was afebrile and had a white blood cell count of 6.7. Blood cultures were sent, and a CT of the abdomen and pelvis demonstrated a large bowel obstruction with a transition point in the left lower quadrant and transverse colon dilation to 9 cm (Figure 1). Blood cultures were negative. The patient’s last colonoscopy was roughly five years prior and was noted to be normal without any biopsies taken. A carcinoembryonic antigen level was also sent, which came back negative.

Figure 1. A: Computed tomography demonstrating a transition point of the large bowel obstruction B: Computed tomography demonstrating 9 cm transverse colon dilation proximal to transition point.
A nasogastric tube was placed, and the patient was made to have nothing by mouth. After adequate intravenous fluid resuscitation and worsening abdominal pain, the patient underwent an exploratory laparotomy. Laparoscopy was considered, but the decision was made to proceed with laparotomy given the degree of colonic dilation. During the operation, the patient was found to have dense adhesions that had obstructed his colon at the splenic flexure. Enterolysis relieved the obstruction, and the colon was decompressed with proctoscopy. After enterolysis, edematous and distended small bowel and colon prevented abdominal closure. A temporary negative pressure dressing was placed, and the patient was transferred to the intensive care unit with ongoing nasogastric and rectal decompression. The patient returned to the OR on postoperative day one for fascial and skin closure.
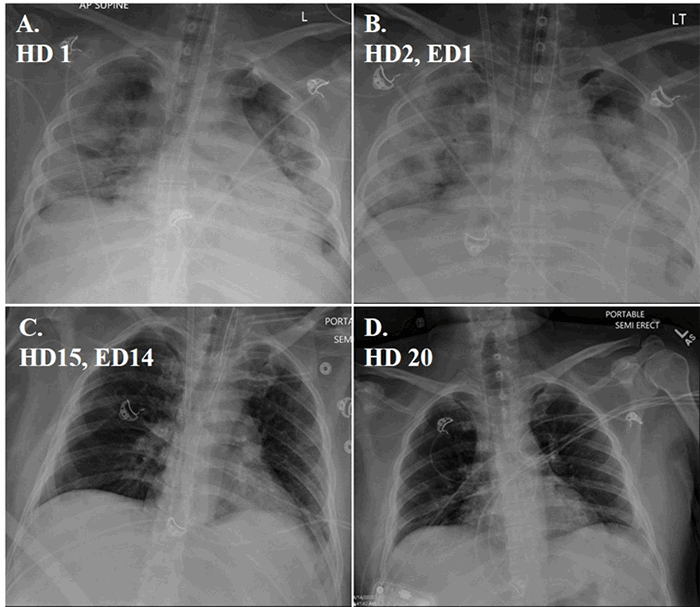
Postoperatively, the patient was extubated and initially did well; however, on postoperative day five, he developed respiratory distress with mixed hypercarbic-hypoxic respiratory failure. A chest X ray revealed a pneumonia and the patient was reintubated. Blood cultures were drawn that grew out salmonella. The patient was initially started on broad-spectrum antibiotics. Sputum cultures grew salmonella, and the patient was subsequently switched to levofloxacin. No changes were made to his immunosuppressive regimen.
During this time, the patient also developed hyperbilirubinemia, which peaked at a total bilirubin of 9.4 mg DL, with a direct component of 6.9 mg DL on postoperative day five. At that time, the patient had an aspartate aminotransferase level of 44, alanine aminotransferase of 15, and alkaline phosphatase level 62. Neither right upper quadrant ultrasound nor hepatobiliary scan identified biliary pathology (Figure 2A and 2B). With no evidence of cholestasis or biliary obstruction, the hyperbilirubinemia was attributed to salmonella hepatitis, and it resolved with treatment of the salmonella infection. The patient was never severely hypotensive during the course of his treatment, making shock liver an unlikely cause of his hyperbilirubinemia. The patient improved on levofloxacin therapy and was eventually weaned and liberated from the ventilator and transferred to a long-term acute care facility.

Figure 2. A: Right upper quadrant ultrasound with normal gallbladder wall and no signs of distention or edema. B: HIDA scan demonstrating filling of gallbladder and duodenum.
Discussion
To the authors’ knowledge, this case is the first documented instance of a large bowel obstruction leading to disseminated salmonellosis. It is illustrative of the complexity typical surgical pathology can assume in an immunosuppressed patient.
This patient had multiple risk factors for enteric infections, including immunosuppression and proton pump inhibitor therapy.1,2 Salmonella species are acid labile, thus an increase in gastric pH allows for increased colonization and risk of infection.3
The immediate inciting factor for the patient’s large bowel obstruction is unclear, as the patient’s only prior abdominal surgery was his kidney transplant, which was done in his right lower quadrant. His history of several days of diarrhea is suggestive of salmonella contributing to the obstruction. Colonic obstructions in children in the setting of salmonella infection have been previously described and are attributed to colonic edema and spasm.4 This complication has not been described in adults. Our patient had a redundant colon at the splenic flexure and extensive adhesions that may have increased his vulnerability to obstruction.
Initial management of colonic obstruction should consist of fluid resuscitation and correction of any electrolyte abnormalities and decompression with a nasogastric tube. For an obstructive process extrinsic to the colon, such as hernia or adhesions, surgical correction should be undertaken. For intrinsic causes of obstruction, either surgical or endoscopic techniques should be considered.5
Bowel obstructions promote the translocation of bacteria.6 This event is particularly common with salmonella due to its ability to survive within macrophages.7 Moreover, the patient’s immunosuppression further increased the risk of bacterial translocation.8 Immunosuppression probably contributed to the severe systemic manifestations of salmonella this patient developed. Patients with long-term steroid use and immunosuppresives from renal transplantation are more likely to present with bacteremia, even in the absence of diarrheal disease. Our patient did not have dysentery, which is likely due to his immunosuppressed state.9,10
Salmonella infection of the respiratory system is uncommon. In a review of 7,779 cases of salmonella infection, only 84 infections (one percent) involved the respiratory system.11 As in our case, salmonella pneumonia is often secondary to enteric or typhoidal infections. In these scenarios, the organism typically reaches the lung through the blood stream as a secondary infection, although inoculation via aspiration is also possible.12 Salmonella pneumonia requires at least two weeks of parenteral or oral antibiotic therapy. Reported mortality rates from salmonella pneumonia in immunosuppressed patients have been reported as high as 63 percent. Prompt and adequate antibiotic therapy is essential.13,14
Salmonella hepatitis has been well-described in the literature and often presents as a diagnostic challenge due to its non-specific clinical and laboratory manifestations. Symptoms can mimic those of viral hepatitis or other infections such as malaria or amebic hepatitis. The most common symptoms are with fever and elevated WBC count,15 but salmonella hepatitis most characteristically manifests with an isolated rise in serum bilirubin without a corresponding increase in transaminases.16 Pathogenesis of hepatic involvement in salmonella infection is not fully understood; however, it is postulated that hepatic dysfunction is due to either direct invasion or to endotoxin-release, leading to immune mediated liver damage.17,18 The clinical course of salmonella hepatitis can be severe with a mortality rate as high as 20 percent in those who receive delayed treatment.19 Fluoroquinolones have been a mainstay of therapy for invasive salmonellosis, however resistance has gradually come an increasing issue. Third generation cephalosporins and azithromycin are increasingly used as a first-line therapy.20
Conclusion
We report a case of a large bowel obstruction leading to bacterial translocation of salmonella and subsequent disseminated salmonella infection complicated by salmonella hepatitis and salmonella pneumonia. Clinicians should be aware of potential risks of bacterial translocation in immunocompromised patients with bowel obstructions.
Lessons Learned
Bacterial translocation can lead to disseminated salmonella via bacterial translocation. For immunocompromised hosts, disseminated salmonella can have multisystem involvement.
Authors
Sanford E. Roberts III, MD
Division of General Surgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA
David D. Aufhauser, MD
Division of General Surgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA
Benjamin M. Braslow, MD
Division of General Surgery, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA
Correspondence
Dr. SE Roberts
3400 Civic Center Ave
Jordan Medical Education Center
Philadelphia, PA
USA 19146
210-274-5828
Sanford.Roberts@uphs.upenn.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102(9):2047-2056; quiz 2057.
- Danziger-Isakov L. Gastrointestinal infections after transplantation. Curr Opin Gastroenterol. 2014;30(1):40-46.
- Bavishi C, Dupont HL. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther. 2011;34(11-12):1269-1281.
- Gross E, Engelhard D, Katz S. Large bowel obstruction: an unusual presentation of salmonella enterocolitis in infancy. Pediatr Surg Int. 2000;16(7):525-526.
- Sawai RS. Management of colonic obstruction: a review. Clin Colon Rectal Surg. 2012;25(4):200-203.
- Sagar PM, MacFie J, Sedman P, May J, Mancey-Jones B, Johnstone D. Intestinal obstruction promotes gut translocation of bacteria. Dis Colon Rectum. 1995;38(6):640-644.
- Wells CL. Relationship between intestinal microecology and the translocation of intestinal bacteria. Antonie Van Leeuwenhoek. 1990;58(2):87-93.
- Crump JA, Sjolund-Karlsson M, Gordon MA, Parry CM. Epidemiology, Clinical Presentation, Laboratory Diagnosis, Antimicrobial Resistance, and Antimicrobial Management of Invasive Salmonella Infections. Clin Microbiol Rev. 2015;28(4):901-937.
- Brown M, Eykyn SJ. Non-typhoidal Salmonella bacteraemia without gastroenteritis: a marker of underlying immunosuppression. Review Of cases at St. Thomas' Hospital 1970-1999. J Infect. 2000;41(3):256-259.
- Cherubin CE, Neu HC, Imperato PJ, Harvey RP, Bellen N. Septicemia with non-typhoid salmonella. Medicine (Baltimore). 1974;53(5):365-376.
- Saphra I, Winter JW. Clinical manifestations of salmonellosis in man; an evaluation of 7779 human infections identified at the New York Salmonella Center. N Engl J Med. 1957;256(24):1128-1134.
- Ingegno AP, D'Albora JB, et al. Pneumonia associated with acute salmonellosis; report of a case of Salmonella bronchopneumonia and 14 cases of interstitial pneumonia. Arch Intern Med (Chic). 1948;81(4):476-484.
- Aguado JM, Obeso G, Cabanillas JJ, Fernandez-Guerrero M, Ales J. Pleuropulmonary infections due to nontyphoid strains of Salmonella. Arch Intern Med. 1990;150(1):54-56.
- Cohen JI, Bartlett JA, Corey GR. Extra-intestinal manifestations of salmonella infections. Medicine (Baltimore). 1987;66(5):349-388.
- El-Newihi HM, Alamy ME, Reynolds TB. Salmonella hepatitis: analysis of 27 cases and comparison with acute viral hepatitis. Hepatology. 1996;24(3):516-519.
- Ahmed A, Ahmed B. Jaundice in typhoid patients: differentiation from other common causes of fever and jaundice in the tropics. Ann Afr Med. 2010;9(3):135-140.
- Khosla SN. Typhoid hepatitis. Postgrad Med J. 1990;66(781):923-925.
- Morgenstern R, Hayes PC. The liver in typhoid fever: always affected, not just a complication. Am J Gastroenterol. 1991;86(9):1235-1239.
- Karoli R, Fatima J, Chandra A, Singh G. Salmonella hepatitis: an uncommon complication of a common disease. J Family Med Prim Care. 2012;1(2):160-162.
- Clark TW, Daneshvar C, Pareek M, Perera N, Stephenson I. Enteric fever in a UK regional infectious diseases unit: a 10 year retrospective review. J Infect. 2010;60(2):91-98.