Discussion
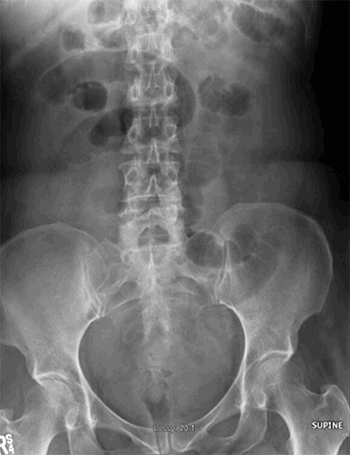
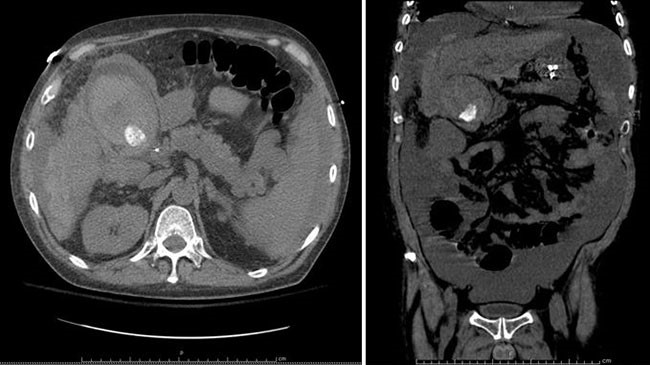
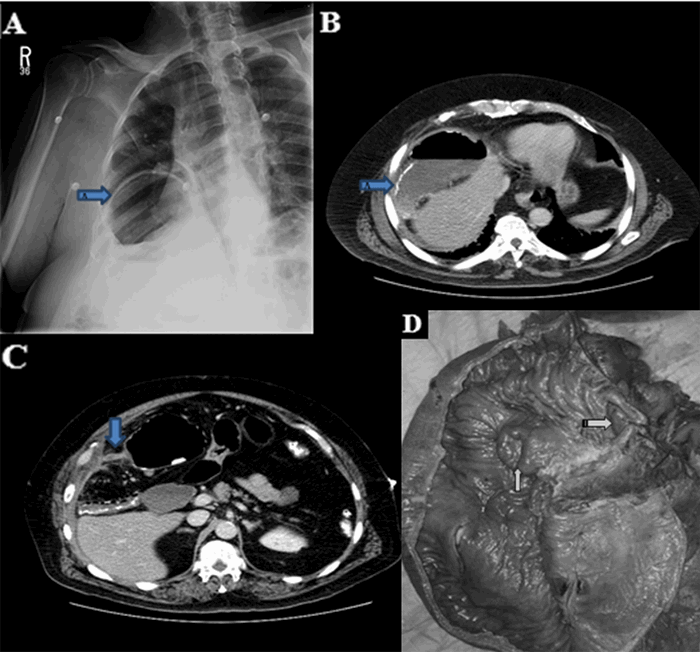
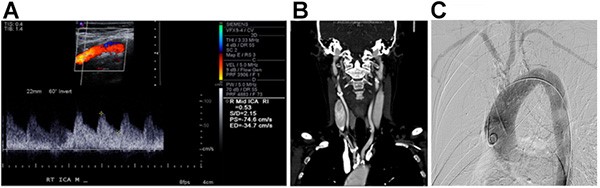
Amoebiasis may range clinically from an asymptomatic carrier state to fulminant colitis and colonic perforation.7,8 E. histolytica infections that cause amoebiasis begin with ingestion of water contaminated with fecal matter containing cysts of the amoeba.9 Trophozoites of the amoeba are released into the lumen of the gastrointestinal tract, where they rapidly clone themselves, leading to formation of new cysts that are excreted in the feces.10 The infection can be located in any part of the intestine, but it is most often found in the cecum and in the ascending colon, as in our case.11 The majority of patients can be managed medically, but a small percentage of patients that have peritonitis require urgent exploration and resection with an associated high mortality rate. About 4 to 10 percent of asymptomatic carriers eventually develop invasive disease.12 Very uncommonly, this disease takes a fulminant course due to the development of necrotizing amoebic colitis; this condition carries a mortality ranging from 55 to 100 percent.13 Occasionally, patients present with tachycardia, hypotension, and peritonitis due to colonic perforation, and urgent intervention is necessary, as in our case study. Fulminant colitis, which is a known variant of amoebic colitis, develops rapidly and presents with features of acute abdomen and loose stools.14 Various risk factors including male gender, increased age, leukocytosis, electrolyte disturbances, and hypoalbuminemia, are associated with the development of fulminant amoebic colitis in patients who have invasive intestinal amoebiasis. Intraoperatively, the fulminating colitis presents as an inflamed, extremely friable colon with underlying full-thickness necrosis and perforation. The colon may be so friable that it can disintegrate with any form of manipulation. Resection of the necrotic colon is the treatment of choice. There is a high risk of suture breakdown in tissue containing amoebae, and exteriorization of the bowel rather than repair is recommended. Despite aggressive surgery, a retrospective analysis of 55 patients with fulminant amoebic colitis was associated with a mortality rate of 89 percent, although in our case, the patient survived and was discharged in a stable state.15,16
Conclusion
Amoebiasis and its complications continue to be a public health problem in developing countries. Cecal perforation may spread to the appendix and lead to gangrenous appendicitis and/or colonic perforation.
Lessons Learned
Even with aggressive management, patients with perforated colon as a result of amoebiasis have a poor prognosis. Resection of diseased segment of colon with exteriorization of bowel is the current gold standard treatment in such cases.
Authors
Kunal Chowdhary
Assistant Professor
Department of Surgery, MMIMSR
Mullana, Ambala, Haryana, India
Abhimanyu Sharma
Senior Resident
Department of Pathology
Mullana, Ambala, Haryana, India
Gurinder Kaur
Postgraduate Student
Department of Anaesthesia
Mullana, Ambala, Haryana, India
Aliya Shah
Postgraduate Student
Department of Microbiology
Mullana, Ambala, Haryana, India
Muzzafar Zaman
Assistant Professor
Department of Surgery, MMIMSR
Mullana, Ambala, Haryana, India
Rahul Yadav
Postgraduate Student
Department of Surgery
Mullana, Ambala, Haryana, India
Ashish Chowdhary
Postgraduate Student
Department of Surgery
Mullana, Ambala, Haryana, India
Ashutosh Bawa
Postgraduate Student
Department of Surgery
Mullana, Ambala, Haryana, India
Correspondence
Dr. Muzzafar Zaman
Department of Surgery
MMIMSR, Mullana,Ambala
Haryana 133207
India
E-mail: muzzafarzaman@yahoo.com
Disclosures
The authors have no conflicts of interest to disclose.
References
- Reed SL. Amebiasis: an update. Clin Infect Dis. 1992;14(2):385-393.
- Matsuura M, Nakase H, Fujimori T, Mizuma K, Tsuda Y, Chiba T. Cecal ameboma. Gastrointest Endosc. 2005;62(3):442-443; discussion 443.
- Stanley SL, Jr. Amoebiasis. Lancet. 2003;361(9362):1025-1034.
- Cox FE. History of human parasitic diseases. Infect Dis Clin North Am. 2004;18(2):171-188, table of contents.
- Gupta SS, Singh O, Shukla S, Raj MK. Acute fulminant necrotizing amoebic colitis: a rare and fatal complication of amoebiasis: a case report. Cases J. 2009;2:6557.
- Majeed SK, Ghazanfar A, Ashraf J. Caecal amoeboma simulating malignant neoplasia, ileocaecal tuberculosis and Crohn's disease. J Coll Physicians Surg Pak. 2003;13(2):116-117.
- Lizcano H DR. Cecal ameboma simulating malignant neoplasiz. Rev Columb Gastroenterol. 2011;26(3):15-18.
- Radovanovic ZL, Katic VV, Nagorni AV, Zivkovic VV, Stankovic TD, Trenkic MS. Clinical diagnostic problems associated with cecal ameboma: case report and review of the literature. Pathol Res Pract. 2007;203(11):823-825.
- Rico H RR. Ameboma do colon ascendente, reporte de caso. Cirugica Generale. 2006;28(Suppl 1):112.
- Ng DC, Kwok SY, Cheng Y, Chung CC, Li MK. Colonic amoebic abscess mimicking carcinoma of the colon. Hong Kong Med J. 2006;12(1):71-73.
- Rouas L, Amrani M, Reguragui A, Gamra L, Belabbas MA. [Diagnostic problems associated with intestinal amoeboma: case report]. Med Trop (Mars). 2004;64(2):176-178.
- Martinez-Paloma A E-CM. Infect Dis. Philadelphia, PA: Elsevier; 2004.
- Guzman V GG, Chavelas Lluck M, Medina Gonzalez E. Unsuspected tumor of the Colon. Rev Gastroenterol Mex. 1996;61:1567-1571.
- Simsek H, Elsurer R, Sokmensuer C, Balaban HY, Tatar G. Ameboma mimicking carcinoma of the cecum: case report. Gastrointest Endosc. 2004;59(3):453-454.
- Hardin RE, Ferzli GS, Zenilman ME, Gadangi PK, Bowne WB. Invasive amebiasis and ameboma formation presenting as a rectal mass: An uncommon case of malignant masquerade at a western medical center. World J Gastroenterol. 2007;13(42):5659-5661.
- Chen H, Hsu YH, Chang YZ. Fulminant amebic colitis: recommended treatment to improve survival. J Thorac Med. 2004;16:1-8.