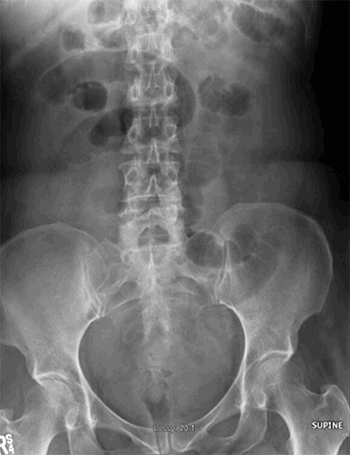
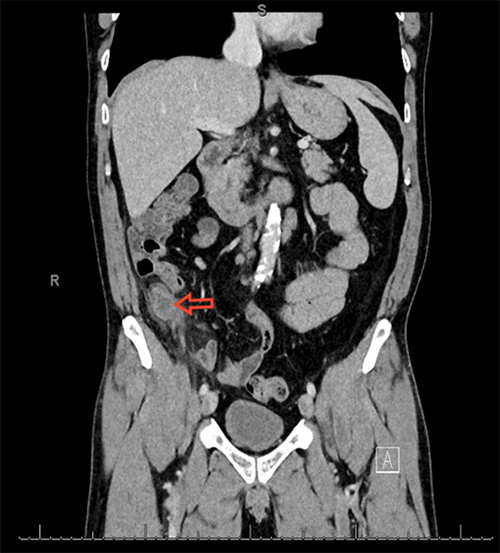
Figure 3. CT of the abdomen and pelvis demonstrating a small bowel obstruction with transition point in the right adnexal region along with stranding of mesenteric fat.
The patient was admitted to the surgical ward and initially managed with bowel rest and intravenous fluids. However, she failed to improve with conservative measures, and therefore was taken to the operating room for diagnostic laparoscopy. After entering the abdomen, the bowel was run retrograde starting at the cecum and progressing toward the ligament of Treitz. This revealed an internal hernia in the right broad ligament that contained incarcerated small bowel. The defect in the broad ligament was medial to the right ovary and inferior to the right fallopian tube. Small bowel was seen entering and exiting this defect with dilated small bowel proximally. The defect in the broad ligament had to be widened in order to reduce the incarcerated small bowel; however, after reduction, the bowel was determined to be viable. Due to concern for future re-herniation, the fallopian tube, ovary, and suspensory ligament were removed, thus opening the entire right pelvic space and permanently and eliminating the risk of recurrence. Following right salpingo-oophorectomy, the hernia defect no longer existed.
The patient was extubated without difficulty and was admitted to the surgical floor. She had rapid return of bowel function and tolerated advancements in diet without issue. She met criteria for discharge on postoperative day two and her entire postoperative course was without complication. She was seen as an outpatient for follow-up two weeks after surgery and was doing well without complaints.
Discussion
Internal hernias are responsible for approximately 0.6 to 6 percent of all small bowel obstructions and are due to congenital or acquired defects.3,4 Hernias through the broad ligament represent four to seven percent of all internal hernias.5 The first reported case of hernia through the broad ligament was discovered via autopsy by Quain in 1861.6 In 1934, Hunt first classified these hernias into three types: the fenestra type, which involves a defect in both peritoneal layers; the pouch type, which involves a defect in one of the two peritoneal layers; and the hernia sac type, which involves the double layer of peritoneum covering the herniated bowel.7 This was followed by Cilley in 1986 with an anatomical classification system for broad ligament defects with three types: type 1 defects occur caudal to the round ligament of the uterus, type 2 defects occur above the round ligament of the uterus, and type 3 defects occur in the mesoligamentum teres of the uterus.8 Potential causes of these defects are obstetrical trauma, prior surgery, and congenital abnormalities.9 Our case represents a hernia sac type according to Hunt's classification and a type 2 defect according to Cilley's classification, a combination that represents the rarest type of herniation through the broad ligament. This case also represents a broad ligament defect that was likely congenital since the patient had no previous surgical or obstetric history. This congenital defect is likely due to incomplete fusion of the paramesonephric ducts during embryonic development.10
No matter the cause of these defects or the classification of these hernias, surgical management appears to be mandatory since every case report published has required surgical correction.11 Surgical management options include suture repair of the defect or salpingo-oophorectomy. Suture repair spares the patient from oophorectomy and is ideal in premenopausal females who desire future fertility. These repairs carry the risk of re-herniation of small bowel through the broad ligament, although more studies are needed to fully understand this complication. Another approach involves salpingo-oophorectomy, which is ideal for postmenopausal women, as in this case. This type of repair eliminates the potential for re-herniation through the defect by completely obliterating the borders of the hernia defect. Both approaches are well tolerated, but further studies are needed to determine long-term outcomes.
Delaying surgical repair can be detrimental to patient outcomes and lead to bowel incarceration or the need for reoperation.12 In case reports by Demir and Redwine, broad ligament defects were noticed on laparoscopy performed for treatment of endometriosis.13,14 In both cases, these defects were left alone and not repaired. Both patients subsequently developed pain after these procedures due to herniation through the unrepaired defects, necessitating reoperation for herniorrhaphy. These reports show that not only is it necessary to surgically repair internal hernias through broad ligament defects, but also that surgeons should consider prophylactic repair if a broad ligament defect is incidentally noticed on laparoscopy. This can help prevent the possibility of future herniation and therefore the need for reoperation.
Conclusion
Internal hernia causing a small bowel obstruction through a broad ligament defect is exceedingly rare, but should be considered in female patients presenting with small bowel obstruction. Early identification of broad ligament defects is crucial to good outcomes since surgical management is required. Prophylactic repair of broad ligament defects should be done when noticed incidentally on laparoscopy to reduce future herniation risk. Laparoscopic management with either suture repair of the defect or salpingo-oophorectomy is safe, effective, and provides excellent short-term clinical outcomes. Long-term follow-up studies are needed to provide evidence based decisions for surgical management of this rare hernia.
Lessons Learned
Internal hernia through a broad ligament defect is very rare. The diagnosis should be considered in women presenting with small bowel obstruction who fail conservative management because surgical intervention is required. Prophylactic repair should be considered if defects are found incidentally in order to prevent hernia occurrence.
Authors
Kenneth Ierardi, RNa,b; Lucas Beffa, MD, FACSb
Correspondence Author
Kenneth Ierardi, RN
Medical Student, University of New England College of Osteopathic Medicine
130 Gano St
Providence, RI 02906
kierardi@une.edu
Author Affiliations
- University of New England College of Osteopathic Medicine, Biddeford, ME
- Kent Hospital, Department of Surgery, Warwick, RI
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Langan, RC, Holzman, K, Coblentz, M. Strangulated hernia through a defect in broad ligament: a sheep in wolf's clothing. Hernia. 2012; 16: 481-483.
- Barbier Brion, B, Daragon, C, Idelcadi, O, Mantion, G, Kastler, B, Delabrousse, E. Small bowel obstruction due to broad ligament hernia: computed tomography findings. Hernia. 2011; 15: 353-355.
- Newsom, BD, Kukora, JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. Sep 1986; 152(3): 279-285.
- Bergstein, JM, Condon, RE. Obturator hernia: current diagnosis and treatment. Surgery. Feb 1996; 119(2): 133-136.
- Karmali, S, Zurawin, RK, Sherman, V. Herniation through the broad ligament. CanMed Assoc J. Feb 2010; 182(2): 174.
- Quain. Case of internal strangulation of a large portion of the ileum. Trans Patholog Soc London. 1861; 12: 103.
- Hunt, AB. Fenestrae and pouches in the broad ligament as an actual and potential cause of strangulated intra-abdominal hernia. Surg Gynecol Obstet. 1934; 58: 906-913.
- Cilley, R, Poterack, K, Lemmer, J, Dafoe, D. Defects in the broad ligament of the uterus. Am J Gastroenterol. May 1986; 81(5): 389-391.
- Ishihara, H, Terahara, M, Kigawa, J, Terakawa, N. Strangulated herniation through a defect of the broad ligament of the uterus. Gynecol Obstet Invest. 1993; 35(3): 187-189.
- Hiraiwa, K, Morozumi, K, Miyazaki, H, Sotome, K, Furukawa, A, Nakamaru, M. Strangulated hernia through a defect of the broad ligament and mobile cecum: a case report. World J Gastroenterol. Mar 2006; 12(9): 1479-1480.
- Garcia-Oria, M, Inglada, J, Domingo, J, Biescas, J, Ching, C. Small bowel obstruction due to broad ligament hernia successfully treated with laparoscopy. J Laparoendosc Adv Surg Tech A.Oct 2007; 17(5): 666-668.
- Baron, A. Defect in the broad ligament and its association with intestinal strangulation. Br J Surg. Jul 1948; 141(36): 91-94.
- Demir, H, Scoccia, B. Internal herniation of adnexa through a defect of the broad ligament: case report and literature review. J Minim Invasive Gynecol. Jan 2010; 17(1): 110-112.
- Redwine, DB. Symptomatic internal hernia of the broad ligament: a complication of electrocoagulation therapy of endometriosis. Obstet Gynecol. Mar 1989; 73(3): 495-496.