Figure 2. A: Hematoxylin and eosin shows keloid-like collagen deposition within a proliferation of spindled fibroblasts. The cells are arranged in short, interlacing fascicles. Extravasated erythrocytes are noted (20x). B: The cells are arranged in a tissue culture-like appearance with myxoid change (20x).
Discussion
Nodular fasciitis is a benign proliferation of fibroblasts and myofibroblasts characterized clinically by its rapid, infiltrative growth and hard consistency, which often leads to suspicion of malignancy, particularly sarcoma.1 This proliferation is thought to be a response to local injury, consistent with its tendency towards spontaneous regression within several months when observed; however, a history of trauma is rarely reported.1,2 Lesions are most frequently identified in soft tissues of the trunk, neck, and extremities.1 Intramuscular and fascial lesions have been described, including one prior report in the pectoralis major fascia and one in the pectoralis major muscle.3,4 No axillary lymphadenopathy or overlying skin changes were observed in cases involving the breast or pectoralis muscle, aiding clinical differentiation from malignant tumors.3-5
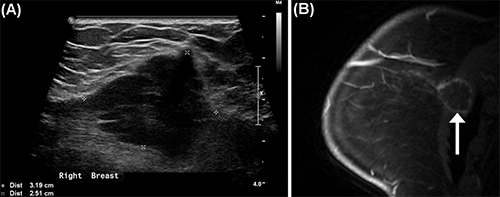
Ultrasound evaluation typically shows a lesion with hypoechoic features, irregular margins, no calcifications, and occasional posterior enhancement and surrounding vascularity.6,7 On CT imaging lesions demonstrate hypoattenuation or iso-attenuation relative to muscle, thus subcutaneous lesions are more well defined than intramuscular lesions. Invasion of adjacent tissue, suggestive of malignancy, is sometimes observed.8 On MRI evaluation, both solid and cystic lesions have been reported, with cystic lesions showing peripheral enhancement and a hyperintense signal on T2 weighted images.8 These imaging features are nonspecific and, combined with clinical features suggestive of malignancy, indicate the need for tissue evaluation. Surgical excision is usually performed because biopsy specimens often do not contain representative cells needed to diagnose nodular fasciitis.3,9
The histologic appearance of nodular fasciitis is typically described as spindle cells in a fascicular growth pattern with mild to moderate inflammatory infiltrate, extravasated erythrocytes, and myxoid and fibrous components.10 A tissue culture appearance of loosely arranged spindle cells with cytoplasmic processes is common.1 Lesions are thought to become more fibrous and less myxoid over time.7 Limited mitotic activity and the absence of nuclear pleomorphism supports the diagnosis of nodular fasciitis over malignant tumors such as fibrosarcoma and leiomyosarcomas. Similar benign lesions such as fibromatosis do not contain the inflammatory elements or show the mitotic activity seen in nodular fasciitis.8,10 Immunohistochemistry is typically positive for smooth muscle actin and negative for cytokeratins, desmin, CD34, and S100.5
Consistent with the existing literature, this case demonstrates the difficulty of differentiating nodular fasciitis from malignant soft tissue tumors prior to observing the characteristic tissue architecture seen in surgical excision specimens. Wide local resection was pursued based on the observed rapid growth, infiltration of adjacent breast tissue seen on imaging, and concern for soft tissue sarcoma based on core needle biopsy findings. Because this clinical course is common, the natural history of the lesion is rarely observed, but a tendency towards spontaneous regression has been described.2 Though most findings are nonspecific in isolation, increased familiarity with the combined clinical, radiographic, cytologic, and immunohistochemistry features of this lesion may aid in determining when to proceed with operative management.
Conclusion
Though benign, nodular fasciitis demonstrates rapid, invasive growth, with nonspecific findings on imaging and core needle biopsy, often suspicious for malignant neoplasm. This case exhibits how these lesions are often not definitively identified until excision is performed. If the benign nature of the lesion can be confirmed prior to operative management and the patient is otherwise asymptomatic, active surveillance may be appropriate.
Lessons Learned
Nodular fasciitis is a rare, benign tumor with a tendency towards spontaneous regression that is frequently excised due to features suggestive of malignancy. With increased familiarity with the features of nodular fasciitis, nonoperative management may be considered.
Authors
Christopher D. Kanner
Medical Student, University of Cincinnati College of Medicine, Cincinnati, OH
Divya Sharma, MD
Department of Pathology and Laboratory Medicine, University of Cincinnati College of Medicine, Cincinnati, OH
Jaime D Lewis, MD, FACS
Department of Surgery, University of Cincinnati College of Medicine, Cincinnati, OH
Correspondence Author
Dr. Jaime D Lewis
UC Health Women's Center
7675 Wellness Way
West Chester, Ohio 45069
Phone: 513-584-8900
Email: lewisjj@ucmail.uc.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Allison DB, Wakely PE, Siddiqui MT, Ali SZ. Nodular fasciitis: A frequent diagnostic pitfall on fine-needle aspiration. Cancer. 2017;125(1):20–29.
- Erickson-Johnson MR, Chou MM, Evers BR, et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91(10):1427–1433.
- Yamamoto S, Chishima T, Adachi S. Nodular fasciitis of the breast mimicking breast cancer. Case Rep Surg. 2014;2014:747951.
- Falco G, Ragazzi M, Cenini E, et al. Intramuscular Nodular Fasciitis of the Pectoralis Major. Breast J. 2016;22(1):122–123.
- Paliogiannis P, Cossu A, Palmieri G, et al. Breast Nodular Fasciitis: A Comprehensive Review. Breast Care (Basel). 2016;11(4):270–274.
- Khuu A, Yablon CM, Jacobson JA, Inyang A, Lucas DR, Biermann JS. Nodular fasciitis: characteristic imaging features on sonography and magnetic resonance imaging. J Ultrasound Med. 2014;33(4):565–573.
- Mazura JC, Matrai C, Spigland N, Brill PW, Kovanlikaya A. Intramuscular nodular fasciitis of the rectus abdominis muscle in an 11-year-old girl. Skeletal Radiol. 2013;42(1):147–150.
- Kim ST, Kim HJ, Park SW, et al. Nodular fasciitis in the head and neck: CT and MR imaging findings. AJNR Am J Neuroradiol. 2005;26(10):2617–2623.
- Samardzic D, Chetlen A, Malysz J. Nodular fasciitis in the axillary tail of the breast. J Radiol Case Rep. 2014;8(5):16–26.
- Squillaci S, Tallarigo F, Patarino R, Bisceglia M. Nodular fasciitis of the male breast: a case report. Int J Surg Pathol. 2007;15(1):69–72.