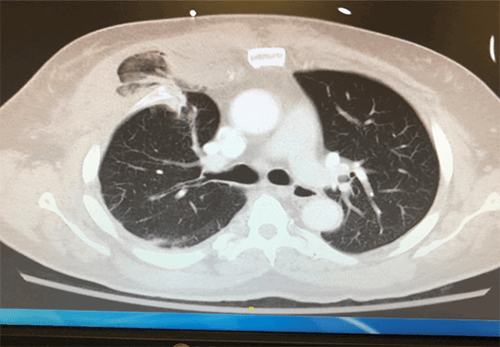
Figure 2. Abdominal X ray of Patient 2 revealing colonic and small bowel dilatation
The patient continued to have persistent colon distension and received a bolus of neostigmine. Two days later, an abdominal X ray showed mild decrease in colonic dilatation. Later that day, a second dose of neostigmine was given with no improvement.
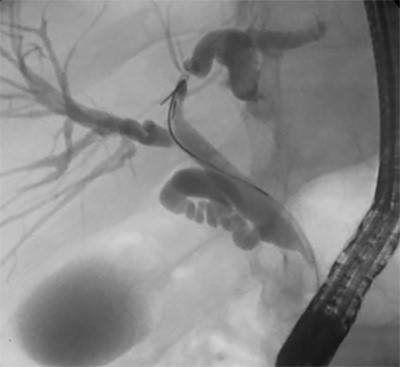
Then colonoscopic decompression was attempted that revealed probable ischemic colitis at the splenic flexure, and this procedure was subsequently terminated due to concern for colonic perforation. The following CT of the abdomen and pelvis revealed no signs of perforation. The next day, abdominal X-ray imaging noted decreased colonic dilatation.
Discussion
The occurrence of Ogilvie syndrome following a stroke is thought to be secondary to autonomic dysfunction,1 likely with excess sympathetic stimulation and parasympathetic inhibition.2 After supportive care, slow intravenous injection of neostigmine is currently the standard of care for treatment of Ogilvie syndrome in new onset and refractory cases.2,3 Neostigmine is a short-acting acetylcholinesterase inhibitor that prevents the degradation of acetylcholine. Thus neostigmine increases parasympathetic activity leading to muscular contraction of the bowel wall by increasing the availability of acetylcholine at the neuromuscular junction for brief periods of time. Patients 1 and 2 both failed multiple neostigmine boluses without trial of other pharmaceutical options. This begs a question: is neostigmine is the appropriate initial treatment for patients with Ogilvie syndrome following stroke?
For cases of pseudo-obstruction that are refractory to boluses of neostigmine, there has been evidence for success using a continuous infusion of neostigmine. It is thought that the continuous infusion allows for the action of neostigmine to persist for longer periods of time to cause sustained stimulation of the bowel to have return of function.2 However, due to the side effects of bronchospasm and bradycardia, continuous infusion of neostigmine should be administered under telemetry in an intensive care unit.2 Alternatively, pyridostigmine has been proven to be effective in treating specifically recurrent cases of pseudo-obstruction.4 Pyridostigmine is a long-acting acetylcholinesterase inhibitor; it is proposed that pyridostigmine is effective in recurrent cases of Ogilvie syndrome because it prolongs the action of acetylcholine even further. Pyridostigmine was shown to be effective in patients with primarily colonic involvement as well as those with additional small bowel dilatation.4
In addition, 5-Hydroxytryptamine (5-HT) receptor 4 agonists such as prucalopride may be efficacious for patients with Ogilvie syndrome. This medication acts by improving peristalsis and causing faster colonic transit leading to more frequent bowel movements.5 In the bowel, 5-HT acts on afferent fibers of the vagus nerve, causing parasympathetic stimulation. Prucalopride has been shown to relieve symptoms of pseudo-obstruction such as bloating, nausea, vomiting, and abdominal pain.5 Prucalopride was observed to be well-tolerated with no significant side effects reported.5
Other literature suggests that the invasive method of colonoscopy for colonic decompression is more successful as the initial treatment for pseudo-obstruction than the current standard of neostigmine. It has been shown that one colonoscopy has greater efficacy requiring no further treatments than even two courses of neostigmine.6 It was found that neostigmine administration prior to colonoscopy did not affect clinical outcomes when compared to no neostigmine given before decompression.6 Colonoscopy was more successful as an initial treatment and in decreasing the need for a second treatment method.7 Perforation is a risk associated with colonoscopic decompression because air insufflation in an already distended colon from large stool volume can cause further distention and increased intra-luminal pressure.7 However, early decompression can lead to prevention of the development of ischemia and perforation.7 This leads us to suggest that colonic decompression may be a more appropriate initial treatment in cases of Ogilvie syndrome secondary to stroke, followed by pharmacological intervention in refractory cases.
Conclusion
Due to the inherent autonomic dysfunction caused by stroke and leading to associated development of Ogilvie syndrome, standard pharmaceutical management does not seem to be the appropriate first-line option. Boluses of neostigmine may not be strong enough in autonomically damaged bowel walls to overcome the dysfunction causing the pseudo-obstruction. Instead, beginning with a continuous infusion of neostigmine, longer-acting acetylcholinesterase inhibitor like pyridostigmine or introduction of an additional bowel motility stimulant with an alternative mechanism of action like prucalopride may provide better relief for this subset of patients due to prolonged exposure and time for effect of the medications. We suggest that colonic decompression with subsequent decrease in tension on the bowel wall, before ischemic damage and/or perforation can occur, may be a more appropriate initial treatment, followed by pharmaceutical treatment in refractory cases of Ogilvie syndrome secondary to stroke.
Lessons Learned
Patients with Ogilvie syndrome occurring after stroke may require initial treatment differing from the current standard of care of a neostigmine bolus for cases of other etiologies. These two cases highlight the potential alternative treatments such as neostigmine continuous infusion, longer acting acetylcholinesterase inhibitors, alternative receptor agonists or colonoscopic decompression. These options may prove more beneficial as first-line therapy for Ogilvie syndrome following stroke due to the inherent autonomic dysfunction caused by stroke.
Authors
Sarah M. Kling, MD
Thomas Jefferson University
Sidney Kimmel Medical College
Philadelphia, PA
Scott D. Goldstein, MD, FACS, ASCRS
Thomas Jefferson University
Sidney Kimmel Medical College
Philadelphia, PA
Correspondence Author
Dr. Scott D. Goldstein
Department of Surgery
Division of Colon and Rectal Surgery
Thomas Jefferson University
1100 Walnut Street
Suite 500
Philadelphia, PA 19107
Phone: 215-570-1464
Email: scott.goldstein@jefferson.edu
Author Affiliations
Thomas Jefferson University
Sidney Kimmel Medical College
Philadelphia, PA 19107
Meeting Presentation
American Society of Colon and Rectal Surgery
Seattle, WA
June 2017
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Wanklyn PD, German A. A case of refractory Ogilvie syndrome following a haemorrhagic stroke. Clin Med. 2013;13:623–624.
- White L, Sandhu G. Continuous neostigmine infusion versus bolus neostigmine in refractory Ogilvie syndrome. Am J Emerg Med. 2011;29:76.e1–3.
- Lee S, Na I, Choi E, et al. Occurrence of intestinal pseudo-obstruction in a brainstem hemorrhage patient. Ann Rehabil Med 2012;36:278–81.
- O'Dea CJ, Brookes JH, Wattchow DA. The efficacy of treatment of patients with severe constipation or recurrent pseudo-obstruction with pyridostigmine. Colorectal Dis 2010;12:540–8.
- Emmanuel AV, Kamm MA, Roy AJ, et al. Randomized clinical trial: the efficacy of prucalopride in patients with chronic intestinal pseudo-obstruction – a double-blind, placebo-controlled, cross-over, multiple n = 1 study. Aliment Pharmacol Ther. 2012;35:48–55.
- Tsirline VB, Zemlyak AY, Avery MJ, et al. Colonoscopy is superior to neostigmine in the treatment of Ogilvie's syndrome. Am J Surg. 2012;204:849–55, discussion 855.
- Peker KD, Cikot M, Bozkurt MA, et al. Colonic decompression should be used before neostigmine in the treatment of Ogilvie's syndrome. Eur J Trauma Emerg Surg. 2017 Aug;43(4):557–566.