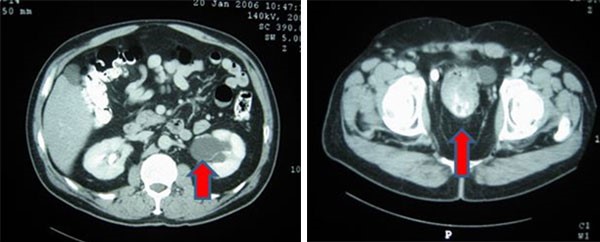
Figure 1. Patient's CT scans. (A): Head CT on arrival to the Emergency Department. (B): Head CT 36 hours later
During the first 24 hours of his admission, the patient was normotensive, ambulating independently without instability, voiding freely, and had normal neurological examinations. The orbital floor fracture was managed nonoperatively. Magnetic resonance imaging (MRI) was negative for acute cervical spine injury. There was no report of a fall or second trauma while hospitalized. Approximately 36 hours after admission, the patient became hypertensive, began complaining of headache and dizziness, and vomited. Upon examination at bedside, he was noted to have an acute change in mental status, with slurred speech, inability to answer questions, and sluggish left pupillary response. An emergency head CT was performed which showed a large, left, near hemispheric subdural hematoma with near complete compression of the left lateral ventricle, and a 1.3 cm left-to-right midline shift with subfalcine herniation (Figure 1). The patient was taken to the OR for an emergent craniectomy with evacuation of subdural hematoma and intracranial pressure monitor placement. Postoperatively, the patient remained critically ill and was admitted to the surgical intensive care unit. Labs were reviewed which revealed a normal coagulation profile (PT, INR and PTT), decrease in platelet count from 163 to 141 x103/uL, and a decrease in hemoglobin levels from 14.2 g/dL to 12.0 g/dL. Postoperatively, GCS persisted at approximately 6-T, and the family elected for tracheostomy, percutaneous endoscopic gastrostomy, and long-term nursing home placement.
Discussion
An acute subdural hematoma (SDH) is a rapidly clotting blood collection below the inner layer of the dura but external to the brain and arachnoid membrane. Delayed acute subdural hematoma is defined as an acute SDH that is not apparent on the initial CT scan but appears on a follow-up CT scan.1 Delayed acute SDH occurs mainly in middle-aged and elderly persons who are either on anticoagulation or antiplatelet therapy. Most of these patients have a GCS score of 15 without loss of consciousness. Neurologic deterioration occurs within the first 24 hours for 70 percent of patients.2 In this article, we describe a case of a healthy adult man, not on anticoagulation or antiplatelet therapy, who presented with a delayed acute SDH 36 hours after a mild head injury.
Livingston et al. published the largest prospective multi-institutional study on the utility of negative CT scans in blunt head trauma.3 In total, 6409 patients were screened at four different level I trauma centers. Patients were included if they suffered from blunt head trauma with GCS of 14 or 15 with loss of consciousness or posttraumatic amnesia. Patients were excluded from the study if on anticoagulants, thrombocytopenic, open or basilar skull fracture, or suffered from cirrhosis, end stage renal disease, severe heart disease, or needed emergent surgery prior to scan. Patients were also excluded from final assessment if the data was incomplete or patient died within 20 hours. Ultimately, 2152 patients were included for final assessment. These 2152 patients underwent initial physical exam, standardized neurologic exam, head CT, and admission for clinical and neurologic monitoring. The patients were monitored for neurologic deterioration, and it was revealed that 1788 patients had head CTs that were officially read as negative. Only five patients with preliminarily negative CT scans required additional neurologic intervention, of which two required increased neurologic monitoring, two required anticonvulsants or anti-edema medication, and one required craniotomy. The craniotomy patient had concurrent facial fractures and required repair of a depressed fracture fragment. The authors conclude a 99.7 percent negative predictive value of a head CT read as preliminary negative in predicting neurosurgical intervention.
af Geijerstam et al. reviewed the literature to investigate the incidence of adverse neurologic outcomes in patients who presented with a negative head CT and specifically a GCS of 15.4 The group conducted an extensive systematic review of multiple publication databases for retrospective studies and case reports which examine the outcomes of patients with an initially negative head CT. Their review included 65,000 patients. Of these, the group was only able to find three documented cases in the available literature of patients who neurologically deteriorated within two days of a normal initial head CT.
In a documented case of delayed acute SDH after a mild head injury in a patient without coagulopathy and normal initial CT findings,5 an 18-year-old-man received a blow to the head during a football game. He did not lose consciousness and did not see a doctor until four days after the injury for complaints of headaches. On the fourth day after the injury, he had a negative neurological evaluation and negative CT imaging. On the eighth day after the injury, he developed neurological sequelae with an emergency CT showing a subdural hematoma with a midline shift. The hematoma was evacuated and the patient made a complete recovery and returned to college.
Conclusion
Our case denotes a unique case of a blunt trauma patient not on anticoagulants or antiplatelets who presented with a GCS of 15 and a CT negative for intracranial hemorrhage, but positive for facial fractures, who approximately 36 hours into his admission acutely deteriorated with devastating neurologic effects. The etiology of his delayed bleed is unknown. While his coagulation parameters were within normal limits, perhaps he had mild coagulation impairment (missed on PT, INR, and PTT) secondary to chronic alcohol consumption, despite only mildly abnormal liver function test results. A more sensitive TEG study may have provided additional information about his clotting function.
Lessons Learned
Delayed acute subdural hematomas after blunt trauma remain very rare in healthy patients who are not on anticoagulants or antiplatelets, with only several cases reported in the literature.
Authors
Philip L. Rosen, MD
SUNY Downstate Medical Center, Department of Surgery, Brooklyn, NY
Daniel J. Gross, MD
SUNY Downstate Medical Center, Department of Surgery, Brooklyn, NY
Fulfilled Ighalo
Richmond University Medical Center, Department of Surgery, Staten Island, NY
Vladimir Rubinshteyn, MD, FACS
Richmond University Medical Center, Department of Surgery, Staten Island, NY
Akella Chendrasekhar, MD, FACS
Richmond University Medical Center, Department of Surgery, Staten Island, NY
Correspondence Author
Dr. Philip L. Rosen
SUNY Downstate Medical Center
Department of Surgery, c/o Dr. Philip Rosen
450 Clarkson Ave, Box 40
Brooklyn, NY 11203
Phone: (718) 270-3302
Email: Philip.Rosen@downstate.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Koyfman A, Radwine Z. Acute Subdural Hematoma in the ED. Medscape website. https://emedicine.medscape.com/article/828005-overview. Updated October, 27 2016. Accessed July 8, 2018.
- Shabani S, Nguyen HS, Doan N, Baisden JL. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016 Dec;96:66–71.
- Livingston DH, Lavery RF, Passannante MR, et al. Emergency Department Discharge of Patients With a Negative Cranial Computed Tomography Scan After Minimal Head Injury. Ann Surg. 2000;232(1):126–132.
- af Geijerstam J, Britton M. Mild head injury: reliability of early computed tomographic findings in triage for admission. Emerg Med J. 2005;22:103–107.
- Matsuda W, Sugimoto K, Sato N, Watanabe T, Fujimoto A, Matsumura A. Delayed Onset of Posttraumatic Acute Subdural Hematoma After Mild Head Injury With Normal Computed Tomography: A Case Report and Brief Review. J Trauma. 2008;65:461–463.