Abstract
Background
Breast cancer is the most common cancer in American women, with increasing age and hormone exposure elevating this risk. However, there are few case reports detailing breast cancer in female-to-male individuals (FTM) receiving masculinizing androgen therapy. Those reports that have been reported have observed younger-age patients after a relatively short duration of hormone therapy. Following a breast cancer diagnosis, it is the standard of care to evaluate for the estrogen receptor (ER), progesterone receptor (PR), and HER2/neu amplification, but androgen receptor (AR) evaluation has not become routine, despite studies showing up to 90 percent co-expression rate in ER-positive tumors. Moreover, the status of these tumor receptors appears to influence the role of AR expression. In vitro studies have shown AR activation in ER-positive tumors can either cause proliferative or anti-proliferative effects depending on ligand and receptor expression levels. In triple-negative tumors, AR expression has been associated with higher rates of metastasis. In HER2-positive tumors, AR stimulation was found to have proliferative effects. Additionally, AR antagonism was found to decrease HER2 activity without changing its expression level.
Summary
A 28-year-old FTM presented with a self-palpated left breast mass after 14 months of weekly testosterone injections for masculinizing effects. Ultrasound-guided core biopsy revealed invasive ductal carcinoma, nuclear grade 3 and ductal carcinoma in situ, nuclear grade 3 with comedonecrosis. Tumor receptors were ER-, PR-, HER2+, Ki67 44.3 percent, and strongly AR positive. He underwent neoadjuvant chemotherapy followed by bilateral nipple sparing mastectomy with left sentinel lymph node biopsy and bilateral transgender chest reassignment.
Conclusion
The safety of androgen therapy in FTMs is uncertain in regards to breast cancer development as well as promoting breast cancer reoccurrence. Our case demonstrates a relatively low-risk individual with neither a family history of breast/ovarian cancer nor genetic abnormalities predisposing one to cancer. Limited reports of breast cancer in FTMs are described in the literature, but this may be a result of the lack of long-term studies as well as many undiagnosed cases due to inadequate cancer screenings or decreased healthcare utilization in this population.
Key Words
Breast cancer, hormone therapy, androgen, transgender
Case Description
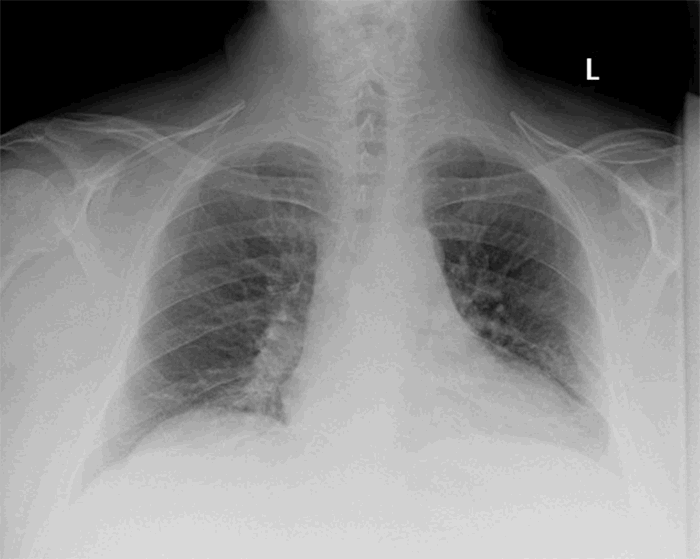
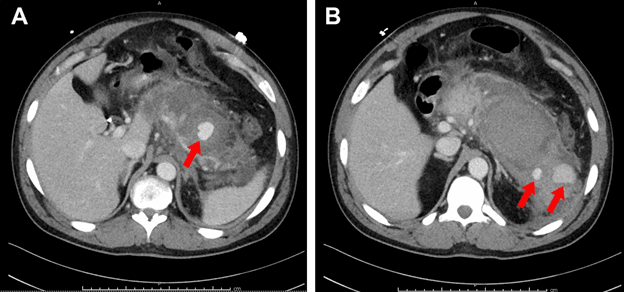
A 28-year-old female-to-male (FTM) patient presented with a self-palpated left breast mass after 14 months of weekly 100 mg testosterone enanthate injections. Ultrasound revealed a hypoechoic mass with indistinct margins in the left breast at 11:00. The mass was bilobed with an anterior portion measuring 14 x 8 x 11 mm and a posterior portion measuring 9 x 7 x 11 mm. The largest dimension of the mass was 24 mm, and the axillary lymph nodes were unremarkable. Ultrasound-guided core biopsy revealed invasive ductal carcinoma (nuclear grade 3) and ductal carcinoma in situ (nuclear grade 3 with comedonecrosis). The tumor was classified as T2N0M0, Stage IIA. The mass was estrogen receptor negative (ER-), progesterone receptor negative (PR-), HER2/neu 3+, Ki67 44.3 percent. Immunostains of the mass revealed tumor cells strongly positive for the androgen receptor. Testosterone therapy was discontinued at the time of diagnosis.
A thorough family history revealed no breast or ovarian cancer within three generations, but there was a history of stomach cancer in both of the maternal grandparents as well as bone and lung cancer in the maternal grandfather and paternal grandmother, respectively. Genetic testing detected no mutations except a variant of undetermined significance for CDH1 and NBN. The patient received four rounds of neoadjuvant treatment consisting of docetaxel (Taxotere), carboplatin (Paraplatin), trastuzumab (Herceptin), and pertuzumab (Perjeta) followed by bilateral nipple sparing mastectomy with left sentinel lymph node biopsy. At the same time, the patient underwent bilateral transgender chest reassignment with bilateral superiorly based fasciocutaneous flaps with bilateral inferior based nipple-areolar complex dermatocutaneous flaps. Final pathology revealed persistent DCIS (3 mm) without evidence of residual invasive cancer. Four sentinel nodes were negative for malignancy. The patient then began IV Herceptin therapy every 23 days and resumed testosterone therapy two weeks following surgery. However, the testosterone was quickly discontinued after a risk discussion, and the patient is currently without evidence of disease.
Discussion
Breast cancer is the most common cancer in American women, with increasing age and hormone exposure increasing risk.1 However, few case reports detail breast cancer in FTM individuals. Compared to natal women, the reported cases of breast cancer in FTM patients receiving masculinizing androgen therapy have been observed at a younger age and after a relatively short duration of hormone therapy (12–24 months).2 Although reports of breast cancer in transgender patients appear to be low, this data may be skewed by many factors. First, risk assessment should always be performed prior to initiating hormone therapy, but there is currently no consensus on screening recommendations. As this patient with a negative family history and genetic screening demonstrated, additional screening factors may need to be considered.3, 4 Furthermore, cases have shown breast cancer in FTMs following bilateral mastectomy for chest reassignment, as these often leave residual breast tissue. Unfortunately, most physicians are not adequately trained in transgender care since it is not a part of most medical school and residency curricula; thus, many physicians may be unaware of how to assess a transgender patient’s cancer risk and properly educate these patients.2,5 This may lead to fewer screenings and delays in diagnosis. Second, fear of discrimination may lead to decreased health care utilization and cancer screenings—leading to potentially undiagnosed cases.3,4
Third, there are no long-term studies on the effects of lifetime hormonal therapy in the transgender population.
In vitro studies have also failed to provide adequate information on which to base clinical decisions. Whereas evaluation for the ER, PR, HER2/neu amplification, and proliferation marker Ki-67 is standard in breast cancer, androgen receptor (AR) evaluation has not become routine despite studies showing up to 90 percent co-expression rate in ER+ tumors.6 Interestingly, the role of AR expression appears to vary with the status of other tumor receptors. In vitro studies have shown AR activation in ER+ tumors can either cause proliferative or anti-proliferative effects depending on ligand and receptor expression levels.6,7 In triple negative tumors, AR expression has been associated with higher rates of metastasis.7,8 In HER2+ tumors, AR stimulation was found to have proliferative effects. Additionally, AR antagonism was found to decrease HER2 activity without changing its expression level.9
Understanding the role of the AR in breast cancer development is not the only area of concern. It is also imperative that we understand the relationship between androgens and breast cancer in order to understand how to properly manage transgender patients with a history of breast cancer. There are concerns regarding restarting androgen therapy due to fear of recurrence. However, permanent discontinuation of hormone therapy can significantly impact not only a patient’s quality of life, but also on their safety. It was been well-documented that the transgender population has high rates of suicide ranging from 32 percent to 50 percent.10 It is essential that we understand how to safely manage these patients during their transition.
In summary, more studies are required to fully evaluate the long-term impact of androgen therapy. There have been few cases of breast cancer reports focusing on FTM patients, but these have been observed to occur at younger ages and in patients who appear to be low-risk. Reporting these types of cases is imperative to guiding future research that will help shape effective screening recommendations and clinical decisions, which will in turn lead to the highest quality of life for these patients.
Conclusion
The safety of androgen therapy in FTMs is uncertain with regards to breast cancer development as well as promoting breast cancer reoccurrence. Our case demonstrates a notable example of a relatively low-risk individual with neither a family history of breast/ovarian cancer nor genetic abnormalities predisposing one to cancer. There are limited cases of breast cancer in the FTM population reported in the literature, but this may be due in part to the lack of long-term studies in this cohort as well as many undiagnosed cases because of inadequate cancer screenings or decreased health care utilization in this population.
Lessons Learned
Androgen therapy may increase one’s risk of breast cancer development. Reports of similar cases and further research are essential to understanding this relationship and how it affects medical and surgical management of this patient population.
Authors
Britney Harris, BS
West Virginia University
Department of Surgery
Morgantown, WV
Aaron Mason, MD
West Virginia University
Department of Surgery
Morgantown, WV
David Borgstrom, MD
West Virginia University
Department of Surgery
Morgantown, WV
Hannah Hazard-Jenkins, MD
West Virginia University
Department of Surgery
Morgantown, WV
Correspondence
David C. Borgstrom, MD
Department of Surgery
1 Stadium Drive
Morgantown WV 26505
E-mail: dcborgstrom@hsc.wvu.edu
Disclosures
The authors have no conflicts of interest to disclose.
References
- U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (1999–2015): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute Web site. www.cdc.gov/cancer/dataviz. Published June 2018. Accessed May 5, 2019.
- Gooren L, Bowers M, Lips P, Konings IR. Five New Cases of Breast Cancer in Transsexual Persons. Andrologia. 2015;47:1202–1205.
- Pivo S, Montes J, Schwartz S, et al. Breast Cancer Risk Assessment and Screening in Transgender Patients. Clin Breast Cancer. 2017;17(5):e225–e227.
- Unger CA. Care of the Transgender Patient: A Survey of Gynecologists' Current Knowledge and Practice. J Womens Health. 2015;24(2):114–118.
- Nikolic DV, Djordjevic ML, Granic M, et al. Importance of Revealing a Rare Case of Breast Cancer in a Female to Male Transsexual after Bilateral Mastectomy. World J Surg Oncol. 2012;10(1):280.
- Basile D, Cinausero M, Iacono D, et al. Androgen Receptor in Estrogen Receptor Positive Breast Cancer: Beyond Expression. Cancer Treat Rev. 2017;61:15–22.
- Christopoulos P, Vlachogiannis NI, Vogkou CT, Koutsilieris M. The Role of the Androgen Receptor Signaling in Breast Malignancies. Anticancer Res. 2017;37(12):6533–6540.
- Mcghan LJ, McCullough AE, Protheroe CA, et al. Androgen Receptor-Positive Triple Negative Breast Cancer: A Unique Breast Cancer Subtype. Ann Surg Onc. 2013;21(2):361–367.
- He L, Du Z, Xiong X, et al. Targeting Androgen Receptor in Treating HER2 Positive Breast Cancer. Sci Rep. 2017;7(1):14584.
- Virupaksha HG, Muralidhar D, Ramakrishna J. Suicide and Suicidal Behavior among Transgender Persons. Indian J Psychol Med. 2016;38(6):505–509.