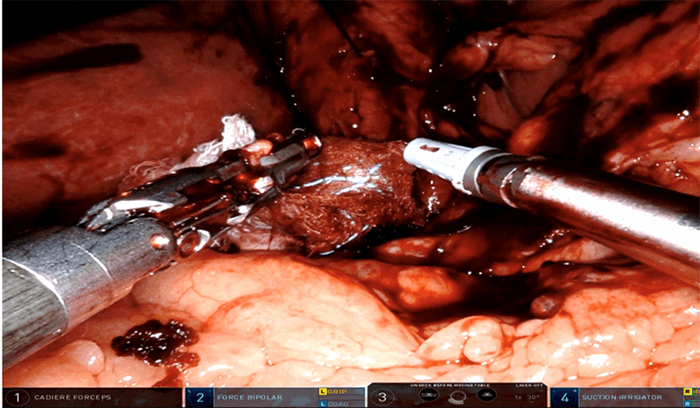
The abdomen was entered via a midline incision to facilitate a thorough exploration. No manifestations of bleeding, perforation, or sustained ischemia were apparent. Focusing on the known pathology to assess for ischemia, we identified a part of the ascending colon that was not in the lesser sac and traced it in the direction of the cecum until we noted rapid tapering of the bowel as it entered the lesser sac via the foramen of Winslow. The cecum and terminal ileum were incarcerated and would not reduce with gentle traction. The lesser sac was entered by hemostatically dividing the gastrohepatic ligament with an intent to apply an additional vector of force to facilitate reduction of the incarcerated bowel. The cecum, terminal ileum, and associated mesentery were dilated and congested, and the vermiform appendix was present; however, no manifestations of ischemia or necrosis were present.
Absent vascular compromise and perforation, we had no indication for resection. We then proceeded with reduction of the hernia, which was accomplished easily after gentle finger dilation of the foramen of Winslow and both careful traction and pressure. The bowel remained viable and mesenteric pulses remained present. While slightly elongated, the ascending colon and adjacent mesentery were not excessively redundant. Incidental appendectomy was performed due to potential difficulty with exposure should interval appendicitis develop. Cecopexy was then performed. We sutured the cecum at several points to the anterolateral peritoneal surface to reduce chances of recurrent internal hernia or volvulus. The remainder of the small and large bowel were evaluated and noted to be absent visible or palpable pathology. Following uneventful closure, she was extubated and transferred to the recovery room.
The patient tolerated the surgery well and was discharged on postoperative day one. She returned to clinic four weeks later and was doing well with minimal pain, ambulating without difficulty, and tolerating a regular diet.
Discussion
There have been only 200 total cases of foramen of Winslow hernia (FWH) since it was first described in 1834 by Bland.1 They are exceedingly rare, representing just 8 percent of internal hernias and only 0.1 percent of all hernias.2 This presents a relative unfamiliarity and challenging diagnosis for even the most experienced physicians where improper diagnosis can result in significant morbidity and mortality.
There are several predisposing pathophysiologic explanations for a FWH. This includes factors involving the foramen itself such as an abnormally enlarged foramen or a defect in the gastrohepatic ligament.3 Others have also commented on factors related to the bowel such as a freely mobile caecum without proper adherence to the peritoneum or an abnormally elongated small bowel mesentery.3
The clinical presentation is often vague and can mimic other hernias or abdominal pathology. Due to the broad differential associated with these symptoms, clinical diagnosis of FWH can be extremely challenging. Due to the potential for incarceration, strangulation, volvulus, and ischemia, delay in surgical management is associated with significant morbidity and mortality. Review of case reports and series indicates delays in diagnosis and treatment has resulted in mortality rates approaching 50 percent.4
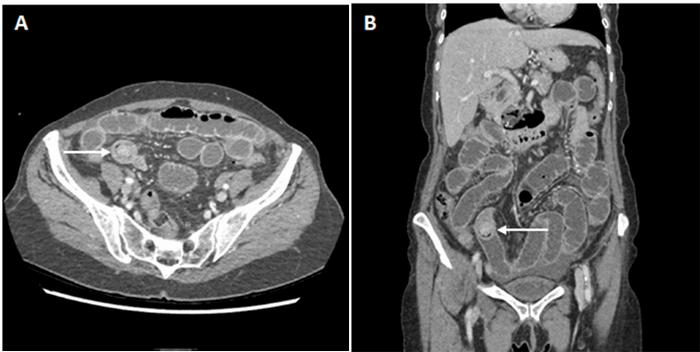
Abdominal pain with obstructive symptoms often prompts surgical consultation leading to axial imaging. Imaging findings include the presence of gas or bowel in the epigastric area that does not fit with the normal contour of the stomach, leftward displacement of the stomach and the duodenum, and failure to visualize the cecum.5,6,7 CT findings include air-fluid levels between the liver hilum and inferior vena cava, anterolateral displacement of the stomach, absence of the ascending colon, and presence of bowel between the portal vein and the inferior vena cava (Figure 2). Treatment requires surgical reduction of herniated contents. Historically the most common surgical approach is a laparotomy, though recently, laparoscopic reduction in experienced hands, has been demonstrated with increasing frequency.5,8 Closure of the hernia defect is not necessary for FWH as a recurrence in the same patient has never been reported.8