Based on the above examinations, a final diagnosis of multiple mesenteric lymphangioma with celiac disease was made. The patient is presently on gluten free diet (GFD) and is symptomatically better at ten months follow-up. A review MRI abdomen was done, which did not show any progression of remaining mesenteric lesions.
Discussion
Cystic lesions of the mesentery are uncommon and their differentials include mesenteric lymphangioma and mesenteric lymph node cavitation. Mesenteric lymphangiomas account for <1 percent of these lesions.2 They are most commonly congenital but may be seen in young adults. Abdominal trauma, lymphatic obstruction, inflammatory process, surgery, or radiation therapy are some causes of a secondary mesenteric lymphangioma.3,4 The patients may be asymptomatic, or present with abdominal pain, due to compression of adjacent small bowel. Uncommonly they may present with acute abdomen due to torsion of the intestine around it, obstruction, secondary infection, rupture or hemorrhage.5
Mesenteric lymphangiomas are commonly an isolated disease process. To the best of our efforts, we could find only one case report in the available English literature published by Miele et al. in 2007, who reported the presence of cystic lymphangioma (CL) and hyposplenism in a case of celiac disease. They concluded in their article that although an association between CL and celiac disease cannot be suggested, a differential diagnosis of CL may be considered for cystic mesenteric masses in patients with celiac disease.6
Mesenteric lymph node cavitation (MLNC) is seen in celiac disease and tuberculosis (TB). TB represents multiple caseating lymph nodes seen in small bowel mesentery and may be associated with other features of abdominal TB, like bowel wall thickening and ascites. Both of these carry different prognoses and treatment options with them. MLNC in celiac disease occurs late in the natural history of the disease and may represent an advanced disease, poor responsiveness to gluten free diet and carry a poor prognosis.7 Empirical ATT for six to nine months, without a clinically defined endpoint of treatment, is often prescribed in peripheral healthcare facilities of many developing countries where tuberculosis is endemic to such patients without an affirmative diagnosis. Such treatment is not particularly beneficial to the patients and it should not be a routine practice.
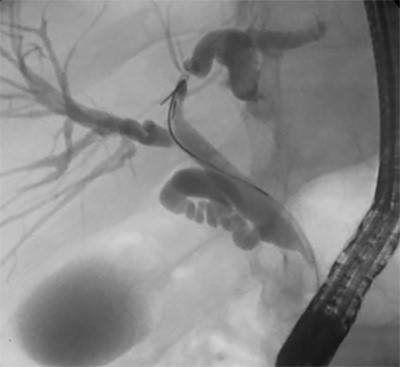
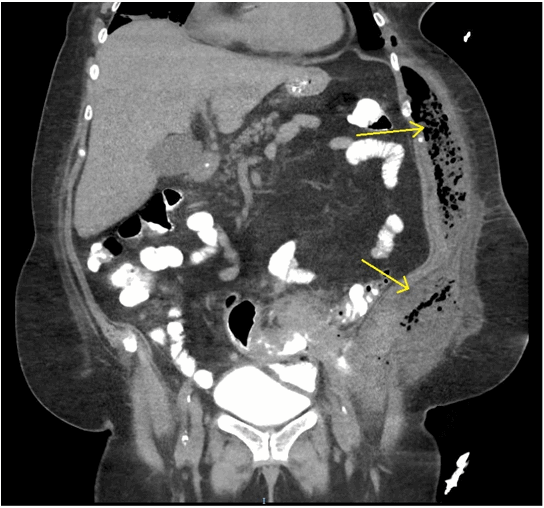
Preoperative diagnosis of mesenteric cystic lesions can be accomplished by imaging with USG showing multiseptated cystic lesions and MRI helping to accurately determine the distribution and characterization.
Conclusion
Mesentric lymphangioma may be rarely associated with other pathologies. A detailed clinical workup is necessary in each case guided by patient’s clinical profile to give him maximum symptom relief.
Lessons Learned
Our case reports a young adult with multiple mesenteric lymphangioma with celiac disease, anemia, and autoimmune hepatitis. Apart from a rare combination of events, this case highlights the role of a detailed and appropriate work up before starting a patient on empirical antitubercular treatment especially in endemic countries.
Authors
Suhani, MS, FACS
Assistant Professor
Department of Surgical Disciplines
All India Institute Of Medical Science (AIIMS)
New Delhi, India
E-mail: druhani@gmail.com
Rajinder Parshad, MS,DNB
Professor and surgical unit head
AIIMS
Department of Surgical Disciplines
New Delhi, India
E-mail: drrajinder.parshad@gmail.com
Ankur Goyal, MBBS, MD
Assistant Professor
AIIMS
Department of Radio-diagnosis
New Delhi, India
E-mail: ankurgoyalaiims@gmail.com
Prasenjit Das, MBBS, MD
Associate Professor
AIIMS
Department of Pathology
New Delhi, India
E-mail: prasenaiims@gmail.com
Raju Sharma, MBBS, MD
Professor
AIIMS
Department of Radio-diagnosis
New Delhi, India
E-mail: raju152@yahoo.com
Govind K. Makharia, MBBS, MD
Professor
AIIMS
Department of Gastroentrology & Human nutrition
New Delhi, India
E-mail: govindmakharia@gmail.com
Correspondence
Dr. Rajinder Parshad
Room number 5035, Teaching Block
Department of Surgical Disciplines, AIIMS, New Delhi
Phone: 011-26593462
E-mail: drrajinderparshad.aiims@gmail.com
Disclosures
The authors have no conflicts of interest to disclose.
References
- Huppert BJ, Farrell MA, Kawashima A, et al. Diagnosis of cavitating mesenteric lymph node syndrome in celiac disease using MRI. Am J Roentgenol. 2004;183:1375-137.
- Jang JH, Lee SL, Ku YM, An CH, Chang ED. Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean J Radiol. 2009;10:319–322.
- Hardin WJ, Hardy JD. Mesenteric cysts. Am J Surg. 1970;119:640–645.
- Daniel S, Lazarevic B, Attia A. Lymphangioma of the mesentery of the jejunum: report of a case and a brief review of the literature. Am J Gastroenterol. 1983;78:726–729.
- Suthiwartnarueput W, Kiatipunsodsai S, Kwankua A, Chaumrattanakul U. Lymphangioma of the small bowel mesentery: A case report and review of the literature. World J Gastroenterol. 2012;18(43):6328 –6332.
- Miele L, Pierconti F, Forgione A, et al. Cystic lymphangioma of the mesentery and hyposplenism in celiac disease. Eur J Gastroenterol Hepatol. 19.11 (2007): 1026 –1030.
- Freeman HJ, Chiu BK. Small bowel malignant lymphoma complicating celiac sprue and the mesenteric lymph node cavitation syndrome. Gastroenterology. 1986;90:2008–2012.
- Stoupis C, Ros PR, Abbit PL, Burton SS, Gauger J. Bubbles in the belly: imaging of cystic mesenteric or omental masses. Radiographics. 1994 Jul;14(4):729 –37.