Mother and fetus tolerated the surgery without complications. Cyclosporine and adalimumab were discontinued and intravenous steroids were transitioned to an oral steroid taper. The patient was discharged home on the 11th postoperative day after resolution of postoperative ileus. Her postoperative course was complicated by recurrent prolapse of the efferent limb of the loop ileostomy that required multiple local reductions with and without anesthetic.
The patient underwent elective cesarean section of a healthy boy at the 36th week of gestation with reduction of recurrent loop ileostomy prolapse. Six weeks post-partum, she again developed recurrent prolapse of the efferent ileostomy limb requiring local conversion to an end ileostomy with closure of the efferent ileostomy limb. At three postpartum months, she underwent total proctocolectomy with ileal pouch anal anastomosis (IPAA) and diverting loop ileostomy with eventual loop ileostomy reversal four months after creation.
Discussion
UC is a disease process that affects a young patient population with peak incidence during reproductive years. An estimated 30–50 percent of female patients with UC will experience an exacerbation while pregnant or in early postpartum period.1 Recent advances in pharmaceuticals, particularly biologic agents, provide physicians with more medical options, but a small fraction of patients will develop medically refractory disease, hemorrhage, perforation, toxic colitis, or sepsis that requires surgery in the gravid state. While perforation, massive hemorrhage, and toxic megacolon are typically steadfast surgical indications, declaring a patient refractory to medicine requires multidisciplinary input to exhaust all options deemed safe for the mother and fetus.
If possible, non-urgent surgery should be performed in the second trimester when preterm contractions and spontaneous abortion are least likely. However, recent consensus guidelines state a pregnant woman should never be denied indicated surgery, regardless of trimester.2 Surgery during pregnancy for UC has historically been a challenging issue with high risk for mother and fetus.3 Preterm delivery, low birth weight, and “small for gestational age” are adverse fetal outcomes associated with active UC during conception or pregnancy.4 A systematic review of 4,473 gravid patients undergoing non-obstetric surgery revealed an overall miscarriage rate of 5.8 percent, but approached 11 percent for women in the first trimester. Premature delivery occurred in 8.2 percent of patients and non-obstetric surgery induced delivery in 3.5 percent of patients, and overall fetal loss rate was 2.5 percent in this cohort of mostly dated studies involving acute appendectomy and cholecystectomy.5 Since maternal gestational weight gain is a strong predictor of adverse pregnancy outcomes in inflammatory bowel disease (IBD)6 the entire surgical care team must show equipoise when deciding on performing surgery during pregnancy.
Restorative proctocolectomy with IPAA (e.g., “J-pouch”) is the ultimate goal for most UC patients requiring surgery, but pelvic surgery during pregnancy is typically avoided given bleeding risks arising from an engorged pelvic venous plexus and the gravid uterus which hinders visualization.7 Moreover, a staged approach to restorative proctocolectomy is typically employed in urgent and emergent settings or in the setting of potent immunosuppressives to minimize postoperative septic complications. Considering the additional nuances associated with pregnancy, surgical options for the gravid UC patient include subtotal colectomy with end ileostomy, partial colectomy with colostomy and mucous fistula, loop ileostomy, and Turnbull colostomy with diverting ileostomy via laparoscopy or open approaches.
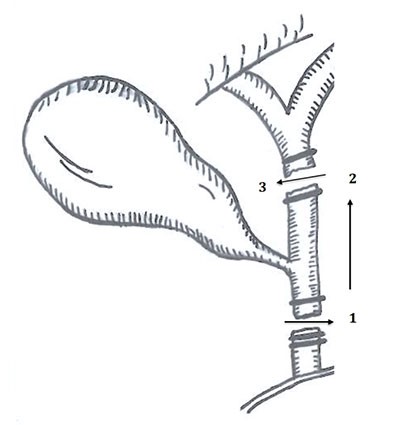
Turnbull first described combined diverting loop ileostomy and decompressive “blow hole” transverse colostomy in 1971 to treat severely ill UC patients with toxic megacolon8 which was later adapted for pregnant UC patients requiring colectomy.9 The “blow hole” colostomy decompresses the colon to avoid immediate resection, and loop ileostomy diversion allows colonic inflammation to gradually improve. Following fetal delivery and maternal convalescence, restorative proctocolectomy can later be completed with lower risk to mother and child under more favorable conditions.
Spartan studies guide optimal surgical management for pregnant UC patients requiring surgery. Wilson et al. reported 38 cases of UC requiring surgical intervention during pregnancy. Sixty percent of patients underwent surgery during the second trimester, and approximately 40 percent of patients had surgery in conjunction with cesarean section.3 Dozois and colleagues reported five pregnant women with fulminant UC who required surgery in the second trimester (3 of 5), first trimester (1 of 5) and third trimester (1 of 5).10 All patients underwent subtotal colectomy and end ileostomy with zero maternofetal mortality and the majority of patients underwent eventual IPAA. The authors proposed using the Turnbull procedure for severely ill and unstable pregnant patients while using subtotal colectomy with ileostomy for all others. Killeen and colleagues later published a systematic review of 56 pregnant UC patients requiring surgery, detailing an overall maternal mortality rate of 19 percent; however, the maternal mortality rate in patients after 1980 was nil.7 The authors noted a fetal mortality of 35 percent, and overall rates of preterm labor approached 50 percent, while all third trimester patients universally experienced preterm labor. While the fetus in the index case was viable at 29 weeks, the authors favored a staged approach utilizing the Turnbull procedure in hopes to minimize the risk of pre-term labor.
Conclusion
Ulcerative colitis exacerbations are commonly encountered during pregnancy and demand coordinated care between gastroenterologists, surgeons, and obstetricians for optimal maternofetal outcomes. Urgent surgery may rarely be required in gravid UC patients and the surgeon must conscientiously balance the immediate well-being of mother and child with a long term surgical strategy to produce a suitable functional gastrointestinal outcome for the mother. Staged surgical approaches, such as the Turnbull blowhole procedure, are helpful adjuncts for high risk UC patients requiring surgery under critical conditions. Elective IPAA procedures can be performed at a later date, when surgery is less perilous.
Lessons Learned
Timeliness of surgical interventions for ulcerative colitis coupled with prudent surgical decision minimizes maternofetal risk during pregnancy. Utilization of staged and temporizing surgeries assures the best long term outcomes for gravid mothers with UC and their fetuses.
Authors
Kelly M. Williamson, MD
Northwestern Memorial Hospital
Chicago, IL
Michael F. McGee, MD, FACS, FASCRS
Northwestern Memorial Hospital
Chicago, IL
Correspondence
Michael F. McGee, MD, FACS, FASCRS
Northwestern Memorial Hospital
251 East Huron Street
Chicago IL 60611
Phone: 312-695-2534
Fax: 312-695-4955
E-mail: mmcgee1@nm.org
Disclosures
The authors have no conflicts of interest to disclose.
References
- Katz JA, Pore G. Inflammatory bowel disease and pregnancy. Inflamm Bowel Dis. 2001;7:146–57.
- Nonobstetric surgery during pregnancy. Committee Opinion No. 696. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2017;129:777–8.
- Wilson IAN, Dench J, Garrett WV. Surgical management of ulcerative colitis in an ongoing pregnancy: report of a case and literature review. Int J Colorectal Dis. 2014;29:271.
- Protic M, Markovic S, Tarabar D. Case Report: Acute Flair of Ulcerative Colitis during Pregnancy Is Still a Major Problem. Dig Dis. 2017;35:134–138.
- Cohen-Kerem R, et al. Pregnancy outcome following non-obstetric surgical intervention. Am J Surg. 2005;190:467–73.
- Bengtson MB, Martin CF, Aamodt G, et al. Inadequate Gestational Weight Gain Predicts Adverse Pregnancy Outcomes in Mother with Inflammatory Bowel Disease: Results from a Prospective US Pregnancy Cohort. Dig Dis Sci. 2017;62:2063–2069.
- Killeen S, Gunn J, Hartley J. Surgical management of complicated and medically refractory inflammatory bowel disease during pregnancy. Colorectal Dis. 2017;19:123–138.
- Turnbull 1971 Turnbull RB, Hawk WA, Weakley FL. Surgical treatment of toxic megacolon. Ileostomy and colostomy to prepare patients for colectomy. Am J of Surg. 1971;122(3):325–331.
- Ooi BS, Remzi FH, Fazio VW. Turnbull-Blowhole colostomy for toxic ulcerative colitis in pregnancy: report of two cases. Dis Colon Rectum. 2003;46(1):111–115.
- Dozois EJ, Bruce WG, Tremaine JW, et al. Maternal and Fetal Outcome After Colectomy for Fulminant Ulcerative Colitis During Pregnancy: Case Series and Literature Review. Dis Colon Rectum. 2005;49:64–73.