Discussion
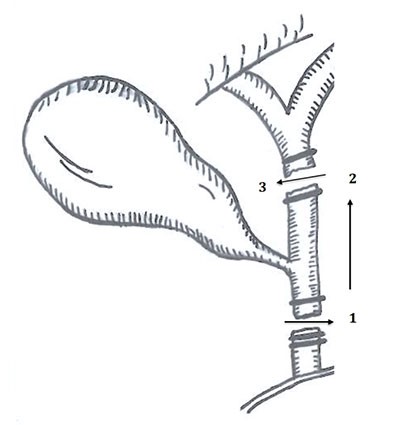
Large vessel leiomyosarcoma is the most common sarcoma arising from blood vessels. It predominately stems from the media of veins rather than arteries, and the large vessel subtype accounts for approximately 2% of all leiomyosarcomas. It is most commonly associated with the inferior vena cava, followed by the venous system of the lower extremities.1 Less than 40 cases of leiomyosarcoma arising from the greater saphenous vein have been reported in the literature. It has an equal female to male predominance and is most commonly diagnosed in the sixth and seventh decades of life, however the age range varies widely (ages 2 to 85 years).2 The tumors tend to develop in an endovascular to exovascular direction. Distant metastasis is identified at the time of diagnosis in approximately 10 to 25% of patients.3
Large vessel leiomyosarcomas of the lower extremity often present late, as soft tissue swelling or mild pain, and can often be misdiagnosed as deep vein thrombosis.4 MRI with gadolinium contrast is the imaging modality of choice for diagnosis. Biopsy techniques should be implored with consideration for standard sarcoma guidelines, including excisional biopsies for small tumors and image guided core needle biopsy or incisional biopsy in the axis of the extremity for larger tumors.2 En bloc surgical resection is the mainstay of treatment and should include margins of at least two to three centimeters.5
The optimal chemotherapy and radiation treatment protocol is poorly studied due to the rare nature of these tumors. Many large vessel leiomyosarcomas are treated with adjunctive radiation therapy; however in tumors less than five centimeters in size it may not be necessary due to the relatively low rate of local recurrence.6 Radiation and its role still largely depends on tumor grade, status of postsurgical margins, and institutional preferences.2 Chemotherapy has not repeatedly shown a clear survival benefit in case series. However, a recent review of the literature reports several recommended regimens which include a combination of doxorubicin and dacarbazapine, or docetaxel and gemcitabine7 all of which have been understudied. While large vessel leiomyosarcoma treatment is vastly understudied due to its uncommon nature, soft tissue sarcoma treatment guidelines have been well established and can be translated to this disease. The National Comprehensive Cancer Network publishes standardized guidelines and include consideration for postoperative external beam radiation and chemotherapy for low grade soft tissue sarcomas with negative resection margins. Multiple different chemotherapy regimens are offered including both previously mentioned.8
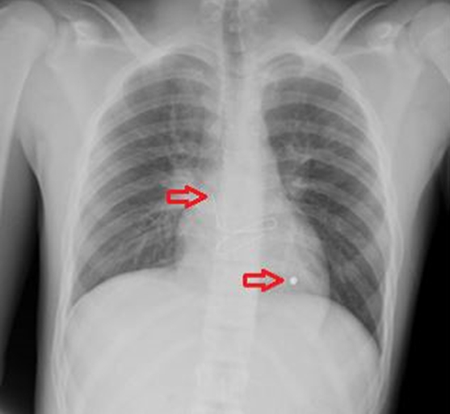
Overall, large vessel leiomyosarcomas have a five-year survival of 25 to 49%, however tumors arising from the IVC have the worst prognosis. Tumors arising from the great saphenous vein have an improved five-year survival of 80 to 90%.2 Recurrence typically occurs within two to three years after completion of treatment and can present as a local recurrence or distant metastasis. Pulmonary metastases are most common.7 Close surveillance throughout this time is recommended, with clinical exams every three months and site-specific MRI and chest X ray recommended every six months.2
Conclusion
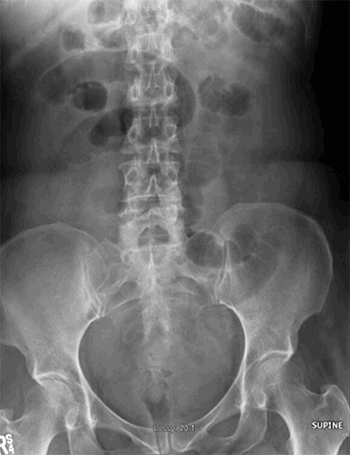
Leiomyosarcoma of the great saphenous vein is an extremely rare tumor arising from the media of the vessel with often indolent symptoms leading to late diagnosis. We present a case of a 43-year-old male with such malignancy after successful resection and a brief review of the recent literature.
Lessons Learned
Large vessel leiomyosarcoma is a rare malignancy most commonly arising from the IVC or veins of the lower extremities. Surgical resection with wide margins is the mainstay of treatment and the most appropriate chemotherapy and radiation protocol has not been well established, but standardized soft tissue sarcoma guidelines can be applied. Close surveillance throughout the first three years after completion of treatment is recommended.
Authors
Kelly Fairbairn, DO
Ventura County Medical Center
Department of Surgery
Ventura, CA
Mrugesh Shah, MD
Ventura County Medical Center
Department of Surgery
Ventura, CA
Javier Romero, MD, FACS
Ventura County Medical Center
Department of Surgery
Ventura, CA
Shawn Steen, MD, FACS
Ventura County Medical Center
Department of Surgery
Ventura, CA
Correspondence Author
Dr. Kelly Fairbairn
Ventura County Medical Center
300 Hillmont Ave
Building 340, Suite 401
Ventura, CA 93003-3099
Email: KFairbairn@cmhshealth.org
Phone: 805-652-5672
Author Affiliations
Ventura County Medical Center
Department of Surgery
Ventura, CA 93003
Disclosure Statement
The authors have no conflicts to disclose.
References
- Erinanc H, Ozulku M, and Terzi A. Recurrence of primary vascular leiomyosarcoma five years after initial diagnosis in the lower extremity. Case Rep Oncol Med. 2018;2018:3094616.
- Cangiano R, Orlandino G, Patitucci G, et al. Primary leiomyosarcoma of the great saphenous vein: case report and review of the literature. Ann Vasc Surg. Jan 2017;38:315.e1-315.
- Bibbo C., and Schroeder M. Review of vascular leiomyosarcoma and report of a case localized to the greater saphenous vein of the ankle. J Foot Ankle Surg. May-Jun 2011;50(3):329-335.
- Zhang M, Yan F, Huang B, et al. Multimodal ultrasonographic assessment of leiomyosarcoma of the femoral vein in a patient misdiagnosed as having deep vein thrombosis. Medicine (Baltimore). Nov 2017;96(46):e8581.
- Dzsinich C., Gloviczki P., van Heerden J.A., et al. Primary venous leiomyosarcoma: a rare but lethal disease. J Vasc Surg. Apr 1992;15(4):595-603.
- Cormier J.N., and Pollock R.E. Soft tissue sarcomas. CA Cancer J Clin. Mar/April 2004;54(2):94-109.
- Italiano A., Toulmonde M., Stoeckle E., et al. Clinical outcome of leiomyosarcomas of vascular origin: comparison with leiomyosarcomas of other origin. Ann Oncol. Sep 2010;21(9):1915-1921.
- von Mehren M., Randall RL., Benjamin RS., et al. Soft tissue sarcoma, version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. May 2018;16(5):536-563.