In regard to the ongoing disease in the neck, the patient later underwent a third neck and mediastinal dissection for metastatic disease in his cervical lymph nodes and a mediastinal lymph node. Subsequent treatment plans for this patient will likely be adjuvant external beam radiation therapy to the neck for palliation followed by another dose of radioactive iodine treatment at 200mCi after thyroid hormone withdrawal to slow the progression of his cervical disease.
Discussion
All type thyroid cancer incidence in the United States is on the rise.1 In papillary thyroid cancer in particular, a recent study cited an incidence increase of 3.5% annually since 1981.2 It is important to note that the papillary type is thought to account for nearly 80% of thyroid neoplasms.3 Papillary carcinoma tumors are classified as having a mixture of both follicular and papillary structures, including overlapping nuclei, longitudinal grooves, and invaginations of cytoplasm in the nuclei.4 This increase in incidence cannot be explained by over diagnosis alone as there has been a significant, yet less hasty incidence of advanced stage and larger primary tumor size papillary thyroid cancers with associated increased mortality rates.2
These neoplasms are often indolent, yielding a 10-year mortality rate of less than 7%.5 Common localized metastases occur through spread to the lymphatics of the thyroid and to regional lymph nodes as well. The mortality rate of distant metastases of papillary thyroid carcinoma is reported as roughly 50%.6 These distant metastases are known to routinely present in the bone or lungs but are rare and only occur in about 2% of patients with papillary thyroid carcinoma.7 Metastasis to tissues other than the bones or lungs is extremely rare. The prognosis of patients with distant metastases is determined by a number of factors, including patient age, tumor grade, size, metastatic site, ability to concentrate, and appearance on chest X ray.8,9 The histologic type of papillary carcinoma is also of utmost importance as certain variants are notably more aggressive. The tall cell variant is observed to more frequently present with lymphovascular invasion, extrathyroidal extension, and distant metastases.10,11 It has a disease-free survival rate that is at least 10% less than classic papillary thyroid carcinoma.12
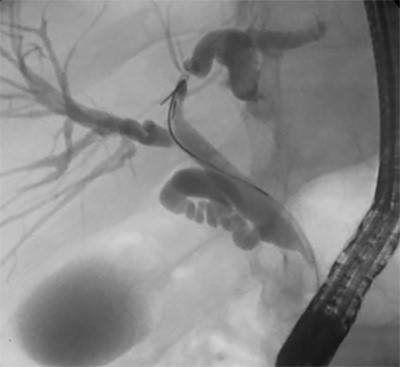
Thyroid carcinoma metastasis to the adrenal gland is very uncommon and few cases are reported in the literature for patients diagnosed with papillary thyroid carcinoma.13-15 Following thyroidectomy, patients have opted for both adrenalectomy with radioiodine therapy, or radioiodine therapy alone. Patients with easily resectable and/or isolated adrenal metastases are good candidates for adrenalectomy. This patient met the criteria for an adrenalectomy with an isolated adrenal metastasis in the setting of presumed lung disease. 18F-fluorodeoxy glucose positron emission tomography/ computed tomography (18F-FDG PET/CT) has become a more common imaging modality in the setting of negative radioiodine scans and elevated thyroglobulin levels.16 FDG PET in our case indicated a right adrenal enhancement and multiple pulmonary nodules, indicative of adrenal malignancy and pulmonary metastases, respectively. Prior to the patient’s right adrenalectomy, thyroglobulin levels were elevated to 149 pmol*L-1, far greater than the 20 pmol*L-1 level which is significantly associated with the presence of residual disease.17 Papillary thyroid carcinoma metastases are generally recommended to be treated with surgical resection as deemed appropriate for the patient’s wellbeing. Previously, resectability has been performed only in isolated metastases. If resection can be performed successfully, patients can experience prolonged survival, increasing five-year survival from roughly 10 to 24%.18
Conclusion
A 61-year-old male who presented initially with unremitting pharyngitis, dysphagia, and a palpable neck mass who was found to have papillary thyroid cancer of the tall cell variant which metastasized to cervical lymph nodes, mediastinal lymph nodes, the lungs, and lastly the right adrenal gland confirmed on FDG-PET imaging. The patient underwent total thyroidectomy, several neck dissections, a mediastinal dissection, and lastly laparoscopic right adrenalectomy in addition to radioactive iodine treatment and planned external beam radiation therapy.
Lessons Learned
While most classic papillary thyroid cancer presentations are rather indolent, certain variants such as the tall cell variant, can present in an aggressive fashion with locally advanced disease and more frequent occurrence of distant metastases. There is not yet clear evidence to determine the effect on mortality resection of distant metastases, and more specifically adrenal metastases, will have on survival, as it is a relatively rare occurrence described in few case reports to date. When common imaging modalities are nondiagnostic, FDG-PET imaging is helpful in localizing distant thyroid cancer metastases to uncommon locations, such as the adrenal gland, particularly in the setting of poorly differentiated cancers.
Authors
Whitney A. Wright, MD
Virginia Mason Medical Center Graduate Medical Education Mailstop H8-GME
Seattle, WA
Andrew P. Collins, BS
University of Washington Bothell
Department of Chemistry
Bothell, WA
Adnan A. Alseidi, MD, EdM, FACS
Virginia Mason Medical Center
Division of General Thoracic and Vascular Surgery
6th Floor Buck Pavilion, C6-GS
1100 9th Avenue Seattle, WA
Correspondence Author
Whitney A. Wright, MD
Virginia Mason Medical Center Graduate Medical Education Mailstop H8-GME
1100 9th Avenue
Seattle, WA 98101
Whitney.Wright@virginiamason.org
(406)-490-9978
Disclosures
The authors have no conflicts of interest or financial disclosures.
References
- Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295(18):2164–2167.
- Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in Thyroid Cancer Incidence and Mortality in the United States,1974-2013. JAMA. 2017;317(13):1338–1348. doi:10.1001/jama.2017.2719.
- Hundahl SA, Fleming ID, Fremgen AM, et al. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985e1995. Cancer. 1998;83:2638–2648.
- Schlumberger MJ 1998 Papillary and follicular thyroid carcinoma. N Engl J Med 338:297–306.
- Donohue JH, Goldfien SD, Miller TR, et al. Do the prognoses of papillary and follicular thyroid carcinomas differ? Am J Surg. 1984;148:168–173.
- Elisei R, Molinaro E, Agate L, et al. Are the clinical and pathological features of differentiated thyroid carcinoma really changed over the last 35 years? Study on 4187 patients from a single Italian institution to answer this question. J Clin Endocrinol Metab. 2010;95:1516–1527.
- Shaha AR, Shah JP, Loree TR. Differentiated thyroid cancer presenting initially with distant metastasis. Am J Surg. 1997;174:474–476.
- Hoie J, Stenwig AE, Kullmann G, Lindegaard M 1988 Distant metastases in papillary thyroid cancer: A review of 91 patients. Cancer 61:1–6.
- Yamashita H, Nogushi S, Yamashita H, Murakami N, Watanabe S, Uchino S, Kawamoto H, Nakayama I 1998 Changing trends and prognoses for patients with papillary thyroid cancer. Arch Surg 133:1058–1065.
- Ganly I, Ibrahimpasic T, Rivera M, Nixon I, Palmer F, Patel SG, Tuttle RM, Shah JP, Ghossein R. Prognostic implications of papillary thyroid carcinoma with tall-cell features. Thyroid. 2014;24:662–670
- Axelsson TA, Hrafnkelsson J, Olafsdottir EJ, Jonasson JG. Tall cell variant of papillary thyroid carcinoma: a population-based study in Iceland. Thyroid. 2015;25:216–220.
- Michels JJ, Jacques M, Henry-Amar M, Bardet S. Prevalence and prognostic significance of tall cell variant of papillary thyroid carcinoma. Human pathology. 2007;38:212–219
- Batawil N. Papillary thyroid cancer with bilateral adrenal metastases. Thyroid. 2013;23:1651–4.
- Malhotra G, Upadhye TS, Sridhar E, et al. Unusual case of adrenal and renal metastases from papillary carcinoma of thyroid. Clin Nucl Med. 2010;35:731–6.
- Copland JA, Marlow LA, Williams SF, et al. Molecular diagnosis of a BRAF papillary thyroid carcinoma with multiple chromosome abnormalities and rare adrenal and hypothalamic metastases. Thyroid. 2006;16:1293–302.
- Caobelli F, Quartuccio N, Pizzocaro C, et al. Unusual Adrenal Gland Metastasis in a Patient with Follicular Carcinoma of the Thyroid Evidenced by 18F-FDG PET/CT and Confirmed by Biopsy. Nucl Med Mol Imaging. 2015:49:73–75.
- Hall FT, Beasley NJ, Eski SJ, Witterick IJ, et al. Predictive value of serum thyroglobulin after surgery for thyroid carcinoma. The Laryngoscope. 2003:113:77–81.
- Kim SH, Brennan MF, Russo P, Burt ME, Coit DG 1998 The role of surgery in the treatment of clinically isolated adrenal metastasis. Cancer 82:389–394.