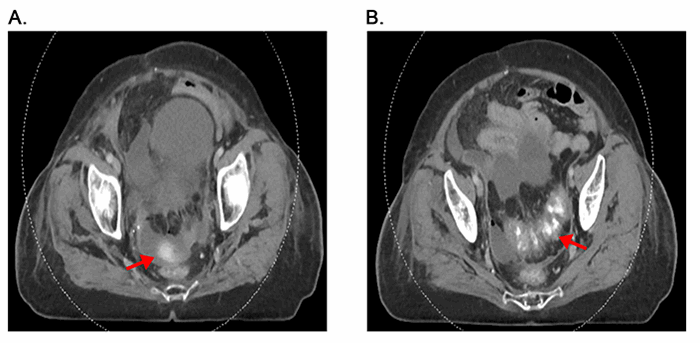
Figure 2. Pathologic analysis indicates immune-mediated colitis. A. Path Low power hematoxylin and eosin (H&E) image showing sigmoid colon with extensive ulceration and full-thickness necrosis extending from the mucosa (arrow) into the muscularis propria (star). B. Medium power hematoxylin and eosin (H&E) image showing colonic glands with acute inflammation, crypt abscesses (arrows), scattered enterocyte apoptosis, and mild lymphoplasmacytic expansion of the lamina propria (star).
Initially, the patient recovered appropriately. She was extubated and had return of bowel function. Immunosuppressive therapy was not continued in the immediate post-operative period due to a concern for impairment in wound healing. However, on post-operative day eight, the patient developed significant hematochezia from her colostomy, had an incomplete response to blood transfusion, and developed hemodynamic instability. She was subsequently taken back to the operating room emergently and underwent completion colectomy to ensure that further complications due to colitis were eliminated. Intra-operatively, an EGD and ileoscopy via enterotomy of the terminal ileum demonstrated normal stomach and small bowel mucosa without evidence of bleeding. Surgical pathology of the removed colon again demonstrated acute inflammation, crypt abscesses and enterocyte apoptosis (Figure 2B). These findings suggest that during the initial operation, more aggressive resection may have been preferable. Post-operatively, the patient had a prolonged hospital course with respiratory failure requiring tracheostomy, extended ventilator management, and she was discharged to a rehabilitation facility. The patient was last seen in surgical clinic at six-month follow-up doing well, having functionally returned to her baseline, and her six-month imaging demonstrated reduction in the size of her largest lung nodules, stable smaller nodules, and no evidence of new lung of abdominal metastases.
Discussion
The advent of immune checkpoint inhibitors has caused a paradigm shift in the treatment approaches for several types of cancer,1,9,14 including lung cancer,15-17 head and neck cancers,18,19 colon cancer,20 renal cell carcinoma,21 urothelial carcinoma,3 and metastatic melanoma.4,6 The combination of a PD-1 and a CTLA4 inhibitor – as used for the patient described in this report – to treat metastatic melanoma has been studied in several large clinical trials.4,6,22 Early trials of monotherapy for advanced melanoma showed that checkpoint inhibitors yielded 3-year survival rates of 20% to 26%,23-28 a significant improvement for a disease with a median survival of eight months and a 5-year survival rate of 10%.29 Subsequent studies of dual-therapy reported that combinations of PD-1 and CTLA4 inhibitors appear superior in terms of overall survival to monotherapy.4-6,30 The outcomes of these clinical trials have been encouraging; however, as the number of patients treated with these agents increases, it is to be expected that the number of patients experiencing severe irAEs will rise accordingly.4,6,31
The incidence of all irAEs has been reported to be 65% and higher for checkpoint inhibitor monotherapy.9,30 This rate is amplified when therapeutics are combined, with rates for adverse events approaching 96% for patients treated with combined nivolumab and ipilimumab compared to 86% for either agent given as monotherapy; severe adverse events of grade 3 or 4 were reported to be 59% for combination therapy, 28% for patients treated with ipilimumab, and 21% for nivolumab treated patients.6 Based on several large clinical trials, the most frequently encountered adverse events include rash, pruritus, fatigue, nausea, and diarrhea, with more severe events such as colitis, pneumonitis, neutropenia, and myelitis occurring much less commonly.4-6,9,12 Most adverse events are minor and can be managed medically. One of the most severe irAEs, colonic perforation, is a rare but well document event and life-threatening in nature.6,31,32
Immune-mediated colitis has been reported to occur in 0.3 to 7% of patients treated with immune checkpoint inhibitors.31 Immune checkpoint-associated colitis most commonly, but not exclusively, affects the rectum and sigmoid colon.8,33,34 When colitis is suspected, immunomodulator treatment should be discontinued immediately, and alternative causes of colitis, such as CMV, IBD, HBV, celiac disease, and Clostridium difficile infection must be excluded.31 The extent of involved colon should be confirmed via flexible sigmoidoscopy or colonoscopy, and biopsies are recommended.8 Immune checkpoint inhibitor-associated colitis tends to differ from inflammatory bowel disease (IBD) in that patients present with acute focal or patchy colitis with infiltrating neutrophils and eosinophils and with crypt abscesses.8 In severe cases, treatment with immune checkpoint inhibitors must be discontinued in perpetuity;.8 in less severe cases, treatment can recommence once symptoms subside: in ipilimumab and nivolumab treated melanoma patients, response rate was not affected by brief periods of treatment discontinuation.31
Medical management for immune-related adverse GI events includes treatment with steroids: corticosteroids given at a fixed dose of 1 mg/kg/day and up to 2 mg/kg/day in refractory or severe cases, followed by a 1-2-month taper once symptoms have improved, has shown good efficacy. Systemic steroid treatment does not seem to negate the anti-tumor activity of checkpoint inhibitors,22,35 but current available data is not entirely conclusive.36 In case of clinical deterioration despite corticosteroid treatment (i.e., no improvement after several days of treatment), infliximab (TNF-α) treatment with a single dose of 5 mg/kg is recommended.31 A second dose of 5 mg/kg of infliximab two weeks after the initial dose should be given if the patient remains symptomatic.
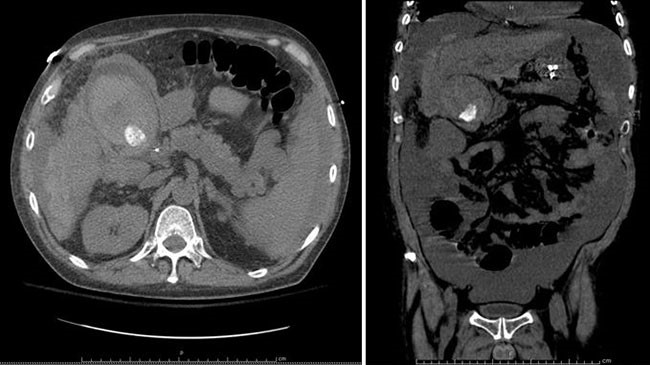
Colon perforation has been estimated to occur in 1.0% to 1.5% of melanoma patients treated with ipilimumab and up to 6% of ipilimumab treated patients with renal cell carcinoma.8,33 There are currently no established molecular markers or host factors to predict adverse events from immunotherapy; although, IL-17, eosinophil levels, neutrophil infiltrates, and other factors are being actively investigated.37 In the case of suspected perforation, CT studies should be completed if the patient is hemodynamically stable; however, in the unstable patient, surgery should not be delayed and exploratory laparotomy is indicated.8 It has not been determined if re-initiation of immunotherapeutic therapy is advisable after surgical treatment.
Post-surgical care of patients that present with colonic perforation after treatment with immunotherapy has not been clearly delineated. Steroid treatment and treatment with infliximab should be considered as options. High-dose corticosteroid administration for less than ten days has not been found to have a significant effect on wound healing; however, chronic corticosteroid use for at least 30 days before surgery increased the risk of complications two to five times.38 Perioperative corticosteroid use or infliximab use for cases of elective surgery for Crohn's disease did not increase rates of early postoperative complications.39 Several additional studies of post-operative use of steroids or infliximab for cases of IBD have shown a small but significant increase in complications, particularly in the rate of infection (intra-abdominal and wound dehiscence).38-40 Despite the small increase in complications, the use of steroids and infliximab may well yield a benefit; in the context of immunosuppression with steroids and/or infliximab, the use of prophylactic measures to reduce the risk of infection requires further investigation.
The case described in this report highlights some of the challenges likely to be encountered by surgeons with increasing frequency as the number of patients receiving treatment with checkpoint inhibitors continues to rise. In the described case, it would have potentially been preferable to perform a colonoscopy intra-operatively to visualize the extent and severity of the inflammation at the initial operation, to determine if the patient would have benefited from a total initial colectomy and/or implement more aggressive treatment with steroids and infliximab post-operatively. Specifics regarding pre- and post-operative management strategies for patients receiving immunotherapy should be explored in future studies.
Conclusion
This case describes one of the most severe adverse events associated with immunotherapy - colon perforation - and discusses the management thereof from a surgical perspective. The enormous success of immune checkpoint inhibitors for the treatment of several different types of cancer is resulting in a steady increase in the number of patients with adverse events requiring surgical intervention. The possibility of colonic perforation should be suspected in patients treated with immunotherapy, aggressive treatment promptly initiated, and early surgical consultation strongly recommended. Further studies are needed to define the cause and optimal treatment paradigm for this complication in this patient population.
Lessons Learned
As the number of cancer patients treated with ICIs increases, the number of patients that experience colonic perforation is expected to escalate as well. It is critical that surgeons are aware of this expanding patient population and of the most appropriate treatment: likely a combination of surgery, steroids and immunosuppression.
Authors
Tim N. Beck, MD, PhD
Digestive Disease & Surgery Institute
Cleveland Clinic
Cleveland, OH
Program in Molecular Therapeutics
Fox Chase Cancer Center
Philadelphia, PA
Yanis Boumber, MD, PhD
Department of Hematology/Oncology
Fox Chase Cancer Center
Philadelphia, PA
Kazan Federal University
Kazan, Russian Federation
Alexander Y. Deneka, MD, PhD
Program in Molecular Therapeutics
Fox Chase Cancer Center
Philadelphia, PA
Kazan Federal University
Kazan, Russian Federation
Emily S. Reardon, MD
Acute Care and Emergency Surgery
University of Maryland Medical Center
Baltimore, MD
Natalie A. O'Neill, MD
Acute Care and Emergency Surgery
University of Maryland Medical Center
Baltimore, MD
Alison O. Flentje, MD
Acute Care and Emergency Surgery
University of Maryland Medical Center
Baltimore, MD
Megan Quintana, MD
Acute Care and Emergency Surgery
University of Maryland Medical Center
Baltimore, MD
Stephanie Richards, MD
Department of Pathology
University of Maryland Medical Center
Baltimore, MD
Brandon R. Bruns, MD, FACS
Acute Care and Emergency Surgery
University of Maryland Medical Center
Baltimore, MD
Paulesh Shah, MD, FACS
Acute Care and Emergency Surgery
University of Maryland Medical Center
Baltimore, MD
Correspondence Author
Tim N. Beck, MD, PhD
Digestive Disease & Surgery Institute
Cleveland Clinic
9500 Euclid Avenue
Cleveland, Ohio 44195
Phone: 216-645-9460
Email: Beckt2@ccf.org
Disclosure Statement
Dr. Boumber has served on advisory boards of Astra Zeneca, Boehringer Ingelheim, Bristol-Meyers Squibb, Caris Life Sciences, Novartis, and Takeda. The authors have no other conflicts to disclose. The authors were supported by the Ruth L. Kirschstein National Research Service Award F30 fellowship (F30 CA180607 [Dr. Beck]) and R01 A218802-01A1 [Dr. Boumber]). Drs. Boumber and Beck were supported by the NCI Core Grant P30 CA006927 (to Fox Chase Cancer Center).
References
- Blumenthal GM, Theoret MR, Pazdur R. Treatment Beyond Progression With Immune Checkpoint Inhibitors-Known Unknowns. JAMA Oncol. 2017.
- Kim ES. Avelumab: First Global Approval. Drugs. 2017;77(8):929-937.
- Powles T, O'Donnell PH, Massard C, et al. Efficacy and Safety of Durvalumab in Locally Advanced or Metastatic Urothelial Carcinoma: Updated Results From a Phase 1/2 Open-label Study. JAMA Oncol. 2017;3(9):e172411.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med. 2015;373(1):23-34.
- Postow MA, Chesney J, Pavlick AC, et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 2015;372(21):2006-2017.
- Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N Engl J Med. 2017;377(14):1345-1356.
- Naidoo J, Page DB, Li BT, et al. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol. 2015;26(12):2375-2391.
- Haanen J, Carbonnel F, Robert C, et al. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv119-iv142.
- De Velasco G, Je Y, Bosse D, et al. Comprehensive Meta-analysis of Key Immune-Related Adverse Events from CTLA-4 and PD-1/PD-L1 Inhibitors in Cancer Patients. Cancer Immunol Res. 2017;5(4):312-318.
- Bertrand A, Kostine M, Barnetche T, Truchetet ME, Schaeverbeke T. Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med. 2015;13:211.
- Kahler KC, Hassel JC, Heinzerling L, et al. Management of side effects of immune checkpoint blockade by anti-CTLA-4 and anti-PD-1 antibodies in metastatic melanoma. J Dtsch Dermatol Ges. 2016;14(7):662-681.
- Boutros C, Tarhini A, Routier E, et al. Safety profiles of anti-CTLA-4 and anti-PD-1 antibodies alone and in combination. Nat Rev Clin Oncol. 2016;13(8):473-486.
- Champiat S, Lambotte O, Barreau E, et al. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol. 2016;27(4):559-574.
- Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409-413.
- Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2016;375(19):1823-1833.
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373(17):1627-1639.
- Bansal P, Osman D, Gan GN, Simon GR, Boumber Y. Recent Advances in Immunotherapy in Metastatic NSCLC. Front Oncol. 2016;6:239.
- Ferris RL, Blumenschein G, Jr., Fayette J, et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med. 2016;375(19):1856-1867.
- Bauman JE, Cohen E, Ferris RL, et al. Immunotherapy of head and neck cancer: Emerging clinical trials from a National Cancer Institute Head and Neck Cancer Steering Committee Planning Meeting. Cancer. 2017;123(7):1259-1271.
- Le DT, Uram JN, Wang H, et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med. 2015;372(26):2509-2520.
- Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N Engl J Med. 2015;373(19):1803-1813.
- Weber J, Thompson JA, Hamid O, et al. A Randomized, Double-Blind, Placebo-Controlled, Phase II Study Comparing the Tolerability and Efficacy of Ipilimumab Administered with or without Prophylactic Budesonide in Patients with Unresectable Stage III or IV Melanoma. Clinical Cancer Research. 2009;15(17):5591-5598.
- Wolchok JD, Neyns B, Linette G, et al. Ipilimumab monotherapy in patients with pretreated advanced melanoma: a randomised, double-blind, multicentre, phase 2, dose-ranging study. Lancet Oncol. 2010;11(2):155-164.
- Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711-723.
- Schadendorf D, Hodi FS, Robert C, et al. Pooled Analysis of Long-Term Survival Data From Phase II and Phase III Trials of Ipilimumab in Unresectable or Metastatic Melanoma. J Clin Oncol. 2015;33(17):1889-1894.
- Hamid O, Puzanov I, Dummer R, et al. Final analysis of a randomised trial comparing pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory advanced melanoma. Eur J Cancer. 2017;86:37-45.
- Petrella TM, Robert C, Richtig E, et al. Patient-reported outcomes in KEYNOTE-006, a randomised study of pembrolizumab versus ipilimumab in patients with advanced melanoma. Eur J Cancer. 2017;86:115-124.
- Schachter J, Ribas A, Long GV, et al. Pembrolizumab versus ipilimumab for advanced melanoma: final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet. 2017;390(10105):1853-1862.
- Garbe C, Eigentler TK, Keilholz U, Hauschild A, Kirkwood JM. Systematic review of medical treatment in melanoma: current status and future prospects. Oncologist. 2011;16(1):5-24.
- Pasquali S, Chiarion-Sileni V, Rossi CR, Mocellin S. Immune checkpoint inhibitors and targeted therapies for metastatic melanoma: A network meta-analysis. Cancer Treat Rev. 2017;54:34-42.
- Prieux-Klotz C, Dior M, Damotte D, et al. Immune Checkpoint Inhibitor-Induced Colitis: Diagnosis and Management. Targeted Oncology. 2017;12(3):301-308.
- Yasuda K, Tanaka T, Ishihara S, et al. Intestinal perforation after nivolumab immunotherapy for a malignant melanoma: a case report. Surgical Case Reports. 2017;3(1):94.
- Gupta A, De Felice KM, Loftus EV, Jr., Khanna S. Systematic review: colitis associated with anti-CTLA-4 therapy. Aliment Pharmacol Ther. 2015;42(4):406-417.
- Marthey L, Mateus C, Mussini C, et al. Cancer Immunotherapy with Anti-CTLA-4 Monoclonal Antibodies Induces an Inflammatory Bowel Disease. J Crohns Colitis. 2016;10(4):395-401.
- Downey SG, Klapper JA, Smith FO, et al. Prognostic factors related to clinical response in patients with metastatic melanoma treated by CTL-associated antigen-4 blockade. Clin Cancer Res. 2007;13(22 Pt 1):6681-6688.
- Min L, Hodi FS, Kaiser UB. Corticosteroids and immune checkpoint blockade. Aging (Albany NY). 2015;7(8):521-522.
- Manson G, Norwood J, Marabelle A, Kohrt H, Houot R. Biomarkers associated with checkpoint inhibitors. Ann Oncol. 2016;27(7):1199-1206.
- Wang AS, Armstrong EJ, Armstrong AW. Corticosteroids and wound healing: clinical considerations in the perioperative period. Am J Surg. 2013;206(3):410-417.
- Colombel JF, Loftus EV, Tremaine WJ, et al. Early Postoperative Complications are not Increased in Patients with Crohn's Disease Treated Perioperatively with Infliximab or Immunosuppressive Therapy. Am J Gastroenterol. 2004;99(5):878-883.
- Nguyen GC, Elnahas A, Jackson TD. The impact of preoperative steroid use on short-term outcomes following surgery for inflammatory bowel disease. Journal of Crohn's and Colitis. 2014;8(12):1661-1667.