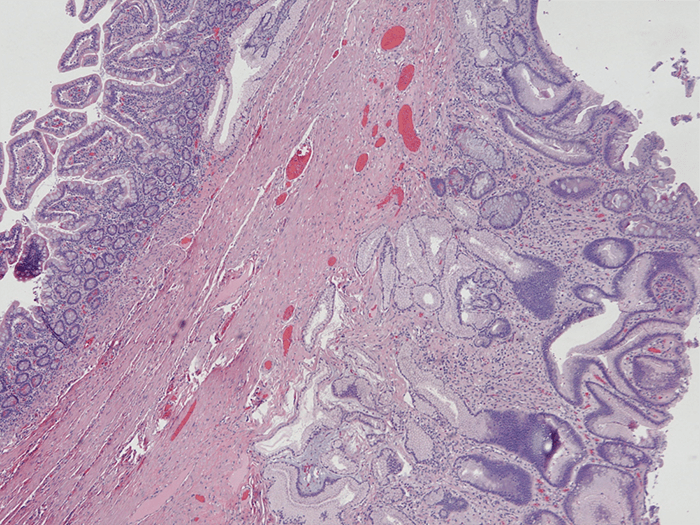
Figure 4. Histology of Resected Small Bowel with Gastric Heterotopia. Normal small bowel mucosa (left) and heterotopic gastric antral type mucosa (right). Hematoxylin & Eosin (H&E) stain, 40x magnification.
Discussion
Tuberculosis can infect the GI tract by hematogenous spread or ingestion. Ingestion of the bacilli and subsequent growth within the lymphoid tissues of the GI tract results in caseous necrosis and ulceration of the overlying mucosa.1 Patients present early in life (21-40 years) with fever, pain, diarrhea or constipation, weight loss, anorexia, and malaise.1 Radiographic findings can vary with disease process and can range from lymphadenopathy and stricture to a frozen abdomen.2 Our patient presented to her physician with fever, abdominal pain, nausea, vomiting, constipation and weight loss and radiographic evidence of multiple strictures. At that time no microbiologic evidence of TB was obtained yet she responded to empiric therapy, and about ten years later a QuantiFERON gold test was positive for TB. These signs and previous habitation within an endemic region makes for a high likelihood of a positive diagnosis. Medical therapy is known to be effective in the treatment of abdominal TB in most cases.3–5 There are however instances in which patients may require surgical intervention for acute therapy to remove actively infected bowel or for more management of remnant stricture disease which we believe was the case in our patient.2
Gastric heterotopia is relatively common finding in the duodenum and proximal jejunum, but somewhat rare in the jejunum.6–8 Gastric heterotopia can be divided into at least two subtypes: congenital and metaplastic. These are differentiated by the presence of multiple histologic subtypes of gastric mucosa, which indicates a congenital origin, versus only antral or pyloric mucosa in metaplastic gastric heterotopia. Meckel's diverticulum is an exception to that rule, as it is a congenital cause but usually contains only antral or pyloric mucosa.6–8 It is thought that metaplastic heterotopia occurs in response to insult and has been seen in conditions such as regional enteritis, tuberculous enteritis, surgical anastomosis, malignancy, radiation and inflammatory bowel disease.9 Lee's paper9 is of particular relevance as he describes six patients who had verified tuberculosis affecting the small bowel, all of whom were females, who had pyloric metaplasia associated with "inflamed or ulcerated mucosa overlying the tuberculous lesion or in the more proximal, obstructed parts of the bowel." Thus, with the known clinical course of our patient and the histology of her stricture, we believe that her stricture was a residual sequalae of intestinal TB.
Stricture disease in intestinal TB occurs during the active phase of the disease and can cause obstructive symptoms in the short or long term. More aggressive evaluation and intervention of her ongoing symptoms, within a year of her original treatment, may have prevented an unnecessarily long course of dietary restrictions and laxatives which our patient endured for nearly a decade of her life. In hindsight, it is important to consider residual strictures from intestinal TB as a possible diagnosis in young otherwise healthy patients who present with symptoms of chronic constipation or intermittent partial small bowel obstructions; especially, in patients who may have had prior exposure to TB. In the absence of such history, pathology may help determine the diagnosis. We believe that, based on the available literature, gastric heterotopia with only antral or pyloric mucosa supports the diagnosis of intestinal TB.
Conclusion
In conclusion we believe our patient suffered from a residual stricture from intestinal TB treated with medical therapy alone. For nearly ten years she was on a puree diet and daily lactulose to prevent the bloating and symptoms of obstruction she would experience with any solid food. Her experience highlights the need for long-term follow up with patients who have been treated for intestinal TB, and that history of TB should be queried when a young otherwise healthy patient presents with obstructive symptoms. A review of the literature suggests that antral type gastric heterotopia may be associated with insult from TB. Our patient is now doing well and on a regular diet.
Lessons Learned
Nonoperative management of intestinal tuberculosis can be effective, but long-term follow up is necessary to ensure complete resolution of symptoms. TB should be considered in patients who may have had prior exposure and present with obstructive symptoms. Metaplastic gastric heterotopia is associated with tuberculous enteritis.
Authors
Alfred S. Song, MD, PhD
Stanford University
Department of Surgery
Stanford, CA
Laura M. Mazer, MD
Stanford University
Department of Surgery
Stanford, CA
Mary T. Hawn MD, MPH, FACS
Stanford University
Department of Surgery
Stanford, CA
Correspondence Author
Mary Hawn, MD, MPH, FACS
Alway Building, Room M121
300 Pasteur Drive, MC 5115
Stanford, California 94305
Phone: (650) 498-4292/(650) 498-7387
Acknowledgements
The authors would like to acknowledge Dr. Allison Jeanne Zemek for her expertise in reviewing the surgical pathology and images that she provided for this article.
Disclosure Statement
The authors have no conflict of interest to disclose, and no funding was required in the writing of this case report.
References
- Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. 2004;120:4:305-315.
- Debi U, Ravisankar V, Prasad KK, Sinha SK, Sharma AK. Abdominal tuberculosis of the gastrointestinal tract: Revisited. World J Gastroenterol. 2014;20:40:14831-14840. doi:10.3748/wjg.v20.i40.14831
- Uzunkoy A, Harma M, Harma M. Diagnosis of abdominal tuberculosis: Experience from 11 cases and review of the literature. World J Gastroenterol. 2004;10:24:3647-3649. doi:10.3748/wjg.v10.i24.3647
- Aggarwal P, Kedia S, Sharma R, et al. Tubercular Intestinal Strictures Show a Poor Response to Anti-Tuberculous Therapy. Dig Dis Sci. 2017;62:10:2847-2856. doi:10.1007/s10620-017-4727-3
- Anand BS, Nanda R, Sachdev GK. Response of tuberculous stricture to antituberculous treatment. Gut. 1988;29:1::62-69.
- Kreuning J, Bosman FT, Kuiper G, Wal AM, Lindeman J. Gastric and duodenal mucosa in "healthy" individuals. An endoscopic and histopathological study of 50 volunteers. J Clin Pathol. 1978;3:1:69-77.
- Wolff M. Heterotopic gastric epithelium in the rectum: a report of three new cases with a review of 87 cases of gastric heterotopia in the alimentary canal. Am J Clin Pathol. 1971;55:5:604-616.
- Owen DA. Stomach. In: Mills SE, ed. Histology for Pathologists. Third. Lippincott Williams & Wilkins; 2006: 589-602.
- Lee FD. Pyloric metaplasia in the small intestine. The Journal of Pathology and Bacteriology. 87:2:267-277. doi:10.1002/path.1700870207