Abstract
Background
A 54-year-old female with a medical history of recurrent anal squamous cell carcinoma treated by abdominoperineal resection develops Bifidobacterium breve bacteremia after an ileal conduit formation complicated by enteric leak.
Summary
Bifidobacterium bacteria is a Gram-positive, nonmotile, branched anaerobic bacteria that is found in the gastrointestinal tract. More recently, it has commonly been used in over the counter probiotic therapies and is a rare cause of anaerobic bacteremia. Our case is a 54-year-old female with recurrent anal squamous cell carcinoma treated with abdominoperineal resection, complicated by radiation cystitis and treated with elective urinary diversion via ileal conduit formation. This was followed by enteric leak secondary to missed enterotomy, for which she required further surgical intervention. The patient's hospital course was further complicated by Bifidobacterium bacteremia. She had no history of probiotic use prior to surgical intervention, and the source of her bacteremia was thus likely due to translocation of bacteria across an impaired gastrointestinal tract barrier or via gross leakage of enteric matter in the setting of missed enterotomy. The patient's clinical condition improved, and cultures became negative after source control was achieved and broad-spectrum antibiotics were utilized.
Conclusion
Bifidobacterium bacteria are a rare cause of bacteremia. The majority of patients who develop bacteremia are less than six weeks of age or greater than 65 years old, and most had gastrointestinal pathology or were immunocompromised. The suspected etiology of these cases of blood stream infection involves bacterial translocation from the gastrointestinal tract resulting in bacteremia. The patient described in this case report matches these characteristics, as she was diagnosed with malignancy and had gross gastrointestinal contamination of her peritoneal cavity. Fortunately, most patients with Bifidobacterium bacteremia recover from their infections. Antibiotics are the main stay of treatment, and a common broad-spectrum regimen was empirically used in this case.
Key Words
Bifidobacterium, bacteremia, postoperative, abdominal surgery
Case Description
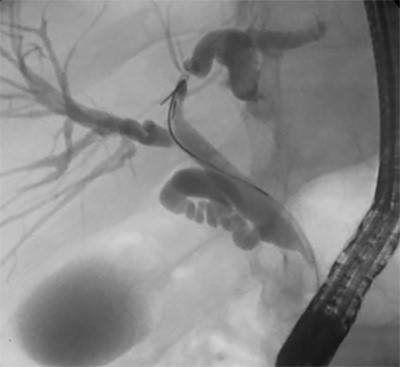
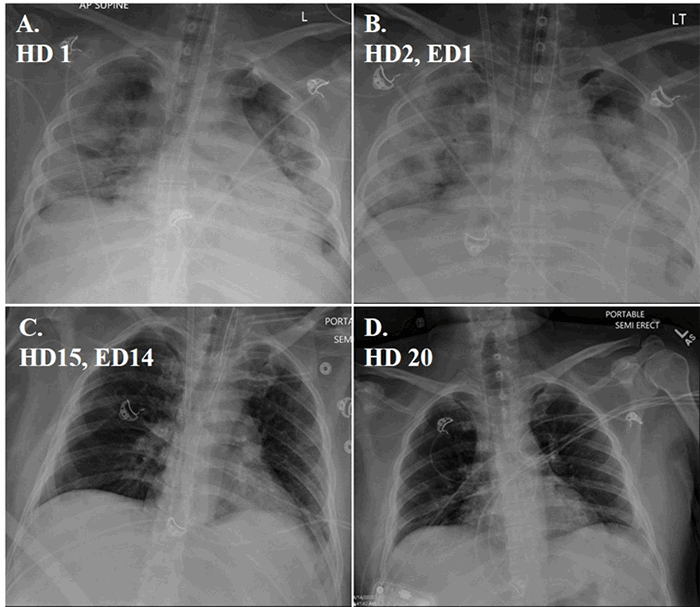
Our patient is a 54-year-old female with a past medical history of diabetes, hypertension, heart failure with preserved ejection fraction, and anal squamous cell carcinoma status post excision and chemoradiation over 20 years prior to presentation. She presented with perineal recurrence 18 months prior to admission and subsequently underwent laparoscopic abdominal perineal resection, posterior vaginectomy, small bowel resection, and end colostomy with a right gracilis rotational flap. Her initial postoperative course was complicated by flap wound dehiscence. Following initial chemoradiation over 20 years before presentation, she had persistent urinary discomfort and incontinence secondary to radiation cystitis. Due to refractory symptoms despite cystoscopy and Botox injections, she elected to undergo urinary diversion by means of cystectomy and ileal conduit formation. The procedure was complicated by dense adhesions and previous pelvic radiation. During the operation, a serosal injury to the terminal ileum was repaired, and a segment of small bowel was resected due to concern for tissue viability. Cystectomy was abandoned as the total cystectomy was difficult to perform. On postoperative day six, her condition deteriorated. She developed respiratory distress, and output in the abdominal surgical drain had a change in character which appeared to be succus. Due to concern for an anastomotic leak, broad spectrum antibiotics were initiated, and she was urgently taken for an exploratory laparotomy. Large volume of succus was encountered in the abdomen, and an enterotomy was discovered within a matted loop of small bowel, deep in the pelvis. The area was resected, and an end ileostomy was matured. The patient was extubated on postoperative day 2, and vasopressors were weaned. Although diagnosed with a contained urine leak, as her abdominal drain had high volume output with elevated creatinine levels, she progressed appropriately. Blood cultures proceeded to grow Bifidobacterium breve. She remained on broad spectrum antibiotic coverage with Vancomycin and Zosyn. Postoperative day 7 coverage was narrowed to only Zosyn, and she was transferred out of the surgical intensive care unit postoperative day 9. Antibiotics were completed post op day 12. Postoperative day 14 she became febrile, and broad-spectrum coverage was restarted. Repeat cultures were only positive for Candida albicans in her urine. Infectious disease was consulted, and she is completing a three-week course of Zosyn and a 10-day course of fluconazole.
Discussion
Bifidobacterium species are common flora of the human gastrointestinal tract, genitourinary tract, and vagina. Despite comprising 80% of a breastfeeding infant's microbiome, and 6 to 8 % of an adult's fecal flora, Bifidobacterium species represent an unlikely cause of bacteremia, accounting for less than 1 to 3% of positive anaerobic blood cultures.1,10 Only 22 cases of Bifidobacterium bacteremia have been reported as of 2015.10
Bifidobacterium, an anaerobic Gram-positive rod, is most commonly known for its use as a probiotic and is frequently given to preterm low birth weight infants to prevent necrotizing enterocolitis (NEC). A 2011 double blind randomized control trial evaluating Lactobacillus casei and Bifidobacterium breve found that probiotic administration reduced the occurrence of NEC.2 Interestingly, therapy with a regime including Bifidobacterium breve was shown to decrease the rates of enterocolitis, pneumonia, and bacteremia in patients with systemic inflammatory response syndrome.7 A meta-analysis of seventeen studies evaluating probiotic's effect on the intestinal mucosal barrier in patients undergoing surgery for colorectal cancer found that probiotics significantly decreased bacterial translocation. The Bifidobacterium to Escherichia ratio, a marker of intestinal flora balance, was significantly improved in patients taking probiotics as well. 4
In the pediatric age group, probiotic use is often present in patients who develop Bifidobacterium bacteremia. Of the 21 patients reviewed by Weber et al, 7 were pediatric patients, all of whom received probiotics.10 A case review of a 2 year old who developed Bifidobacterium breve sepsis in the setting of probiotic supplementation while being treated for high-risk acute lymphoblastic leukemia concluded that current literature is not sufficient to recommend empiric probiotic use in pediatric patients receiving chemotherapy.1
It is known that colorectal surgery alters the patients gut microbiome through iatrogenic factors such as perioperative manipulation, bowel cleanse, antibiotics, and alterations in nutrition.8 In fact, a randomized controlled trial found significantly decreased numbers of Bifidobacterium and total Lactobacillus species in patients who had undergone a mechanical bowel prep compared to patients who had not.9 A trial investigating intestinal microbiome differences in colorectal cancer patient before they began preoperative preparation the day before surgery and post operatively again re-demonstrated a significant decrease in obligate anaerobes including Bifidobacterium and found an increase in facultative anaerobes. Five of the six surgical site infections in that study consisted of species whose counts were increased after surgery, with the one exception being a deep polymicrobial infection.6 Bifidobacterium, a species that is most commonly decreased in number after major abdominal operations, makes our patient's source of infection even more unusual.
Despite the benefits outlined above, Bifidobacterium species represent a rare cause of bacteremia. The isolate in this patient remains even rarer, with Bifidobacterium breve representing 13 to 19% of all Bifidobacterium bacteremia cases.3,10 The prototypical patient afflicted by bacteremia with Bifidobacterium species, as outlined by Esaiassen et al, is a person of extremes of age, who is immunocompromised, with an impaired gastrointestinal barrier. A report evaluating 15 cases of Bifidobacterium sepsis, found that 10 of these patients had gastrointestinal diseases, ranging from metastatic colon cancer to cholecystitis, of which nine had impairment of the intestinal barrier. The patient in this case falls directly into 2 out of 3 of these characteristics, and the source of her bacteremia is most likely due to translocation of the bacteria across her impaired intestinal barrier. In a review of 21 cases, probiotic use was not recorded or unknown in the 15 adult patients with Bifidobacterium bacteremia, compared to 100% of the pediatric patients. This patient once again fits the outlined mold, as she denied any recent probiotic use, or consumption of active live culture-containing foods, such as yogurt or cheese.10
Bifidobacterium was found to have low MICs to Vancomycin and Zosyn. The majority were susceptible to clindamycin as well. In general, these bacteria were resistant to fluoroquinolones.3 A 2005 study investigating 50 strains of 8 species of Bifidobacterium found them to be susceptible to β-Lactams, glycopeptides, and erythromycin. There was no resistance found to penicillin G, amoxicillin, amoxicillin/clavulanic acid, ticarcillin, piperacillin, cefotaxime and imipenem. In general, there were high resistance rates to metronidazole and aminoglycosides. Of note Bifidobacterium breve was found to be more resistant than other Bifidobacterium species.5 Her clinical improvement can be attributed to appropriate use of empiric antibiotic use and obtaining efficient source control.
Conclusion
Bifidobacterium bacteria, a normal flora of the GI tract, is a rare cause of anaerobic gram-positive bacteremia. A common probiotic, it is frequently prescribed in premature pediatric population and cancer patients, who are often exposed before becoming bacteremic. Probiotic use was not noted to be associated in reviewed cases of bacteremia in adult patients. Instead, the bacteremia is believed to be a result of translocation of bacteria across an impaired gastrointestinal tract barrier in immunocompromised and post abdominal surgical patients.
Lessons Learned
Bacteremia with rare or unexpected bacteria species must always remain in the differential diagnosis of a septic patient. This is especially true in immunocompromised patients with impairment of natural barriers of defense. This case underscores the importance of source control and early use of broad-spectrum antibiotics.
Authors
James Walker, MD
University of Texas Southwestern
Department of Surgery
Dallas, TX
Sneha Bhat, MD
University of Texas Southwestern
Department of Surgery
Dallas, TX
Jacqueline Babb, MD
University of Texas Southwestern
Department of Surgery
Dallas, TX
Bonnie C. Prokesch, MD
University of Texas Southwestern
Department of Surgery
Dallas, TX
Kareem R. Abdelfattah, MD
University of Texas Southwestern
Department of Surgery
Dallas, TX
Correspondence Author
Dr. James Walker
UTSW General Surgery Resident
4617 Lorraine Ave
Dallas, TX 75209
404 895 9092
james.walker@phhs.org
Disclosure Statement
The authors have no conflicts of interest or financial disclosures to declare.
References
- Avcin SL, Pokorn M, Kitanovski L, Premru MM, Jazbec J. Bifidobacterium breve Sepsis in Child with High-Risk Acute Lymphoblastic Leukemia. Emerg Infect Dis. 2015;21(9):1674-1675.
- Braga TD, Silva GAPD, Lira PICD, Lima MDC. Efficacy of Bifidobacterium breve and Lactobacillus casei oral supplementation on necrotizing enterocolitis in very-low-birth-weight preterm infants: a double-blind, randomized, controlled trial. Am J Clin Nutr. 2010;93(1):81-86.
- Esaiassen E, Hjerde E, Cavanagh JP, Simonsen GS, Klingenberg C. Bifidobacterium Bacteremia: Clinical Characteristics and a Genomic Approach To Assess Pathogenicity. J Clin Microbiol. 2017;55(7):2234-2248.
- Liu D, Jiang X-Y, Zhou L-S, Song J-H, Zhang X. Effects of Probiotics on Intestinal Mucosa Barrier in Patients With Colorectal Cancer after Operation. Medicine. 2016;95(15).
- Moubareck C, Gavini F, Vaugien L, Butel MJ, Doucet-Populaire F. Antimicrobial susceptibility of bifidobacteria. J Antimicrob Chemother. 2005;55(6):1057-1057.
- Ohigashi S, Sudo K, Kobayashi D, Takahashi T, Nomoto K, Onodera H. Significant Changes in the Intestinal Environment After Surgery in Patients with Colorectal Cancer. J Gastrointest Surg. 2013;17(9):1657-1664.
- Shimizu K, Ogura H, Goto M, et al. Synbiotics Decrease the Incidence of Septic Complications in Patients with Severe SIRS: A Preliminary Report. Dig Dis Sci. 2008;54(5):1071-1078.
- Stavrou G. Gut microbiome, surgical complications and probiotics. Ann Gastroenterol. 2017. 2017; 30(1): 45–53.
- Watanabe M, Murakami M, Nakao K, Asahara T, Nomoto K, Tsunoda A. Randomized clinical trial of the influence of mechanical bowel preparation on faecal microflora in patients undergoing colonic cancer resection. Br J Surgery. 2010;97(12):1791-1797.
- Weber E, Reynaud Q, Suy F, et al. Bifidobacterium Species Bacteremia: Risk Factors in Adults and Infants. Clin Infect Dis 2015;61(3):482-484.