The patient had an uncomplicated postoperative course, with immediate improvement in her abdominal and pelvic pain. She was discharged home but then readmitted to the hospital two weeks later with CHF exacerbation and abdominal wall seroma, which was treated with percutaneous drainage. During her hospital stay she was also treated for mucosal and vaginal candidiasis. She tolerated these treatments well, improved clinically and was discharged home. She followed up in the office six months postoperatively and is doing well with complete resolution of her pelvic pain and no evidence of mass or hernia recurrence.
Discussion
Schwannomas are tumors of mesenchymal origin that arise from peripheral nerve sheath cells.1 These typically benign, solitary, and well-encapsulated neoplasms rarely arise from peripheral nerve fibers, with an estimated prevalence of 1-3%.1,3 Schwannomas more commonly manifest in the head and neck, extremities, mediastinum, and trunk.1 Although schwannomas can occur in all age groups, they are found predominantly in women in the 5th and 6th decades of life.2 Retroperitoneal tumors are rare, but are usually found incidentally. They frequently arise from the paravertebral region in the retroperitoneum, in relation to the nerve of origin, though neurologic symptoms are rare. Clinical presentation may be the result of compression on local structures, and the propensity for these tumors to present at late stages (with compressive symptoms) is a result of the compliance of the retroperitoneal space.1 In this patient's case, it was not clear which was the peripheral nerve of origin, however given its proximity it may have been branches of the femoral nerve, genitofemoral or obturator nerve. In contrast, patients may complain of nonspecific symptoms such as vague abdominal or pelvic pain.
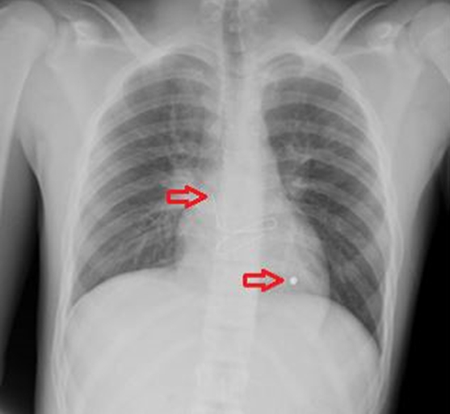
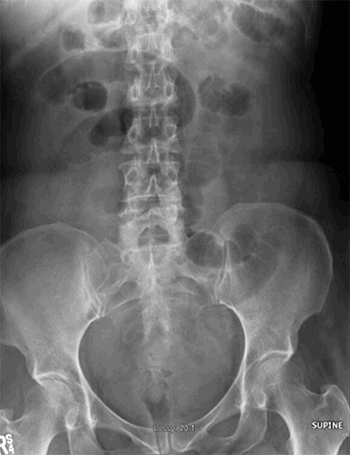
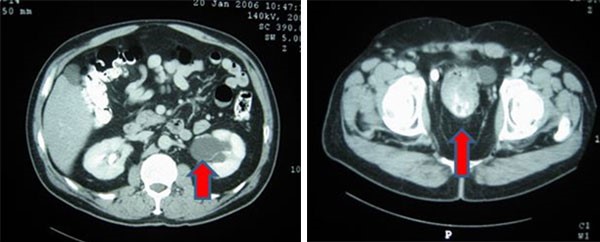
Imaging modalities that may assist with preoperative workup include CT and/or magnetic resonance imaging (MRI). CT scans usually reveal well-defined, heterogeneous lesions and may demonstrate cystic, necrotic, or hemorrhagic components frequently with internal calcification. MRI may be particularly useful in identifying vascular architecture suggestive of malignancy, although this is nonspecific.1 Although some institutions use adjunct final needle aspiration cytology to aid in diagnosis, the varying characteristics of these lesions invariably lower the contribution of the results and such an approach should be limited to centers that have developed specific expertise in these protocols. As a result, core needle biopsies should be obtained as part of the standard diagnostic workup as per the European Society for Medical Oncology guidelines.
Malignant transformation to neurofibrosarcoma is rarely seen, however has been reported to occur following surgical resection of histologically benign schwannomas. The development of malignant changes is more likely to occur in patients with Von Recklinghausen disease.4 Histologic features suggestive of malignant potential include high mitotic count, pleomorphism, and neovascularization.2 Postoperative monitoring with serial surveillance using annual CT scans is recommended to monitor carefully for recurrence or malignancy.1
Complete surgical excision with negative margins is the recommended curative treatment, as postoperative pathology and immunohistochemistry is needed for final diagnosis. In addition, schwannoma responds poorly to radiation and chemotherapy and so adjuvant therapies are not an option. An en bloc excision of adjacent structures may be warranted but was not necessary in this case. The patient's hernia was repaired with synthetic mesh, given the need for tension free repair in the setting of recurrent hernia, and the lack of contamination. Gross examination of schwannomas usually reveal solitary, well-circumscribed, smooth tumors. Histologic features include a biphasic pattern with areas of high (Antoni type A) and loose cellularity (Antoni type B).2,3,4 Nuclear palisading and Verocay bodies are classically seen, although their presence may be variable.2 Tumors show diffuse cytoplasm positivity for S-100 protein.
Conclusion
Our patient had multiple comorbidities that precluded aggressive surgical management of an initially asymptomatic retroperitoneal mass. Interval surveillance allowed for appropriate recognition of mass enlargement, as well as symptoms related to the mass. The development of a large, recurrent, symptomatic incisional hernia necessitated intervention, allowing for concurrent resection of a known retroperitoneal mass.
Lessons Learned
The purpose of serial surveillance is ultimately to determine appropriateness and timing of intervention. Pre-operative diagnosis of retroperitoneal schwannomas is challenging given non-specific radiographic features and low yield of percutaneous biopsies. Definitive management is with surgical excision, which allows for both treatment, and diagnosis with postoperative pathology and immunohistochemistry.
Authors
Monica K Zipple, MD
Department of General Surgery
St Joseph Mercy Oakland
Pontiac, MI
Anna L Shu, DO
Department of General Surgery
St Joseph Mercy Oakland
Pontiac, MI
Sujeivan Mahendram, MS
Department of General Surgery
St Joseph Mercy Oakland
Pontiac, MI
Malik E McKany, MD
Department of General Surgery
St Joseph Mercy Oakland
Pontiac, MI
Correspondence
Monica Zipple, MD
44405 Woodward Avenue
Pontiac, MI 48341
(989) 506-1533
mzipple@gmail.com
Disclosure of Conflicts
The authors have no conflicts of interest to disclose.
References
- Holbrook C, Saleem N. Retroperitoneal schwannoma: an unusual cause of abdominal distention. BMJ Case Reports 2017; 2017: bcr-2017-220221.
- Narasimha A, Kumar H, Kalyani R, Madan M. Retroperitoneal cystic schwannoma: A case report with review of literature. J Cytol 2010; 27(4): 136-139.
- Kapan M, Önder A, Gümüş M, Gümüş H, Girgin S. Retroperitoneal schwannoma. J Surg Case Rep 2011;10: 1–1.
- Goh B, Tan Y, Chung Y, Chow P, Ooi L, Wong W. Retroperitoneal schwannoma. Am J Surg 2006; 192(1): 14–18.