Abstract
Background
In the emergent setting, paraesophageal hernia (PEH) repairs are performed by open laparotomy with gastropexy and/or feeding tube placement, or laparoscopically, depending on the surgeon's expertise. Recently, endoscopic techniques have been developed for high-risk patients. This case demonstrates the importance of preoperative risk assessment in determining which surgical intervention will provide the patient with the most symptom relief and the safest outcome.
Summary
A 90-year-old female with past medical history of symptomatic critical aortic stenosis, coronary artery disease, pacemaker, congestive heart failure, atrial fibrillation on Eliquis, pulmonary hypertension, hypothyroidism, GERD, and hiatal hernia presented to the emergency department with gastric outlet obstruction caused by a PEH. She was evaluated by cardiology, cardiothoracic surgery, internal medicine and anesthesia and was deemed prohibitive risk for definitive surgical repair. The patient successfully underwent endoscopic gastroduodenoscopy (EGD), endoscopic reduction of PEH, and gastropexy with insertion of a percutaneous endoscopic gastrostomy (PEG) tube. She had an uneventful postoperative course and was tolerating a mechanical soft diet prior to discharge. She was discharged to a skilled nursing facility on postoperative day four. At her two-week follow up, she was progressing very well without complication.
Conclusion
Endoscopic reduction and anterior gastropexy with PEG tube placement is a safe and effective method for management of incarcerated PEHs with gastric outlet obstruction in patients who are a prohibitive risk for surgery. This case helps in recognizing the importance of considering all surgical treatment options and weighing the risks and benefits of each when determining a plan of care for an elderly, high-risk patient.
Key Words
Paraesophageal hernia (PEH); gastric outlet obstruction (GOO), elderly; aortic stenosis; endoscopic; high-risk
Case Description
In the aging population, hiatal hernias are due to gradual enlargement of diaphragmatic hiatus. As the defect grows, the intra-abdominal esophagus, stomach, and or other organs can migrate above the diaphragm.1 Hiatal hernias are classified as type I–IV. Type I is a sliding hiatal hernia in which the gastroesophageal junction (GEJ) is displaced above the diaphragm.2 Type II–IV are paraesophageal hernias (PEHs). Type II results in migration of the stomach into the chest without GEJ, and in type III, the GEJ migrates with the stomach into the chest cavity..2 In a type IV PEH, the stomach is displaced into the chest along with other intraabdominal organs.2
Patients with a PEH may be asymptomatic for years, but typical presenting symptoms include chest pain, epigastric pain, heartburn, regurgitation, dysphagia, postprandial fullness, abdominal pain, vomiting, and anemia.1–3 PEHs have the potential to result in gastric volvulus, incarceration, strangulation, necrosis, and/or perforation; therefore, definitive surgical repair is recommended.1
Large type III and IV PEHs are most commonly found in the elderly population, more specifically females.3,4 Due to advanced age, patients have multiple medical comorbidities of varying severity. It is imperative that the operative risks are weighed against the risks of gastric incarceration or strangulation.1 Preoperative risk assessment is of great importance in this aging population, as some patients may deemed prohibitive risk for definitive surgical repair.1,4
The recommended surgical repair for PEH is laparoscopic reduction of the hernia, mobilization of GEJ, repair of diaphragmatic defect, and fixation of stomach within the abdomen with or without anti-reflux procedure such as a fundoplication.1,5,6 In the emergent setting, PEHs are typically repaired by open laparotomy with gastropexy and/or feeding tube placement, or laparoscopically, depending on the surgeon's expertise.3 That said, a few small studies have shown that laparoscopic or endoscopic reduction with gastropexy with or without laparoscopic assistance has been a successful means of hernia reduction and symptom relief in the high-risk, aging population.1,3,6,7 This case demonstrates the importance of preoperative risk assessment in determining which surgical intervention will provide the patient with the most symptom relief and the safest outcome.
In this current case, a 90-year-old female with past medical history of symptomatic critical aortic stenosis (AS), coronary artery disease, pacemaker, right and left heart catheterization, congestive heart failure, atrial fibrillation on Eliquis, pulmonary hypertension, GERD, and hiatal hernia presented to the emergency department with nausea, vomiting, epigastric pain, dysphagia to liquids with regurgitation, and weight loss for two weeks.
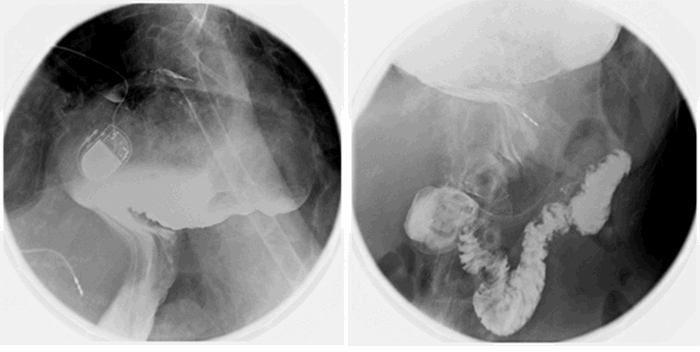
Computed tomography (CT) from outside facility performed earlier in the week revealed gastric outlet obstruction (GOO) caused by a massive type III PEH (Figure 1–4). She was subsequently discharged from this facility as she did not want surgical intervention and opted for hospice care. She presented to the ED later that week for persistent pain. At this time, it was decided to obtain a barium swallow instead of the repeat CT, demonstrating an intrathoracic stomach with concern for underlying gastric volvulus (Figure 5). Due to worsening obstructive symptoms, pain, and evidence of gastric outlet obstruction with possible gastric volvulus, it was recommended she undergo surgical intervention that day.