
Retained Gallstone Presenting as Hepatic Mass
A 49-year-old otherwise healthy female presented with a retained gallstone mimicking a hepatic malignant tumor.
November 27, 2020
Abstract
Background
A 49-year-old otherwise healthy female presented with a retained gallstone mimicking a hepatic malignant tumor.
Summary
A 49-year-old female presented for workup of a suspected liver lesion on background of a previous laparoscopic sleeve gastrectomy and cholecystectomy one year prior. Imaging studies included computed tomography (CT) and magnetic resonance imaging (MRI) of the abdomen confirming a segment six enhancing hepatic lesion suspicious for either a primary liver lesion or a liver metastasis. The patient underwent a laparoscopic segment six liver resection. Histopathology confirmed a diagnosis an inflammatory liver abscess due to a retained gallstone. Although the incidence of retained gallstones is common, the consequences of spillage and unretrieved gallstones have varied presentations. Rarely retained gallstones can develop into inflammatory masses that may mimic soft tissue neoplasia, particularly when there are significant delays to presentations resulting in significant morbidity. Therefore, the diagnosis of complications of retained stones requires a high index of clinical suspicion. As there are limited previous reported cases of this nature, the authors hope to bring to light an uncommon and potentially preventable presentation.
Conclusion
The consequences of retained gallstones are usually associated with an unexpected clinical presentation and can result in significant morbidity. This case highlights stone spillage prevention and the need for complete retrieval of spilled gallstones at the original operation to prevent future sequalae and significant comorbidities.
Key Words
Retained gallstones; hepatic; pseudotumor; liver lesion
Case Description
Laparoscopic cholecystectomy remains the treatment of choice for symptomatic cholelithiasis and is one of the most common surgical procedures in Australia, with 40,326 cases reported from 2017 to 2018.1 The laparoscopic method for cholecystectomy is the preferred technique over the open procedure due to both the lower morbidity and complications for the patients as well as a faster postoperative recovery time.2 However, it has previously reported that laparoscopic cholecystectomy has a higher rate of retained gallstones.3 Gallbladder perforations and spillage of stones is a common intraoperative event that occurs in 5 to 40 percent of laparoscopic cholecystectomies.3 The consequences of this spillage rarely result in subsequent complications.
There are several reports of intrahepatic liver abscess as a result of retained gallstones.3-6 However, there are even fewer reports of patients presenting with a hepatic pseudotumors. Here, the authors present a case of a retained gallstone presenting as a hepatic mass 12 months after an elective laparoscopic cholecystectomy in a 49-year-old healthy female patient.
This patient presented for a suspected liver lesion. Her past medical history was a laparoscopic sleeve gastrectomy and cholecystectomy in June 2017 performed at another institution with minimal operative documentation provided. Intraoperatively, it was noted that she had a nodular-looking liver consistent with nonalcoholic steatohepatitis. The patient’s family history was also significant as her father died from hepatic malignancy.
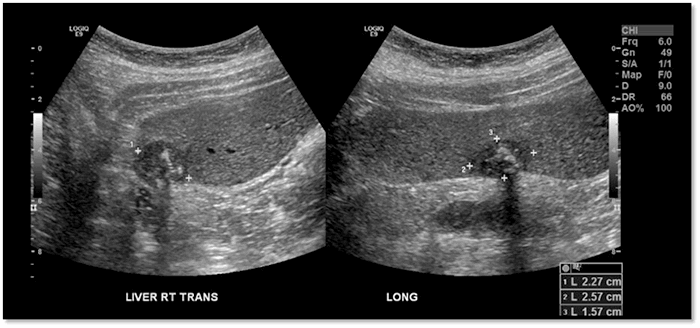
Following surgery, the patient experienced recurrent intermittent vomiting for nine months accompanied by 9 kg weight loss. There was no associated abdominal pain, fevers, or jaundice. Routine bloods showed normal liver function tests as well as normal tumor markers. A liver ultrasound performed in June 2018 demonstrated two hypoechoic lesions with internal calcifications (Figure 1) suspicious for primary hepatic malignancy. Subsequent CT abdomen reported two atypical lesions of possible metastatic disease.
Figure 1. Liver Ultrasound showing hypoechoic lesions with internal calcification in segment six measuring 23 x 26 x 16 mm.
A MRI abdomen performed in July 2018 confirmed a segment six enhancing subcapsular lesion approximately 23 x 22 x 21 mm suspicious for a primary liver malignancy such as hepatocellular carcinoma or a hepatic metastasis (Figure 2).
Figure 2. MRI of patient showing segment six ring enhancing mass.

After discussion with the patient and taking in account her family of a hepatic malignancy as well as the highly suspicious imaging findings, the recommendation was to proceed with a liver resection. The patient underwent a laparoscopic segment six liver resection in September 2018. Intraoperative examination of the specimen demonstrated an inflammatory area of tissue encasing a firm mass suspicious for a retained calculus (Figure 3).
Figure 3. Intraoperative specimen examination of segment 6 liver resection with associated cholelithiasis shown.

Histopathological examination reported a macroscopically nodular area corresponding to abscess formation with the presence of polymorphous inflammatory infiltrate with prominent numbers of neutrophils. Calcified material representing remnants of calculi were also identified, confirming a diagnosis of an inflammatory liver abscess due to a retained gallstone.
Postoperatively, the patient made an uneventful recovery and was discharged four days after the surgery. Routine four-week follow-up with the patient demonstrated a routine complete recovery.
Discussion
Gallstone spillage is common during laparoscopic cholecystectomy and occurs in up to 40 percent of cases.3 Currently, the reported incidence of retained gallstones varies from 1 to 13 percent of operations, with complications of spillage occurring in 0.08 to 2.9 percent of cases.3,7,8 Complications that can arise secondary to retained stones include intraabdominal abscess, abdominal wall abscesses, cutaneous sinus tracts, enteric fistulas, bladder fistulas, and bowel obstruction.6,9,10 Though presentations of retained gallstones are varied, complications can be a major cause of morbidity.
Laparoscopic cholecystectomy for acute cholecystitis remains the most common cause of gallstone spillage.11 This is more common in acute cholecystectomy compared with elective cholecystectomy, as it is likely to have adhesions and inflammation-causing tissues to be more friable and prone to tearing.6
Retained gallstones often lead to local inflammatory responses with local fibrosis resulting in either a mass being walled off by omentum or partial reabsorption.8 Presentations of retained gallstones as hepatic abscesses have been reported in several case reports.3-6 The timeframe of presentations of retained gallstones vary from months to years. Woodfield et. al. found that, on average, the initial presentation occurred at 5.5 months post-laparoscopic cholecystectomy.8 However, diagnosis of retained stone complications can take an additional 4.5 to 4.8 months. Less frequently, a subset of patients can also present years later with retained gallstones mimicking a liver tumor.3,5,9 Cases by Arai et al.,5 Ramohand et al.,3 and Casillas et al.9 outlined patients presenting with an inflammatory mass mimicking a liver tumor developing after four to five years post-cholecystectomy. Casillas et. al. further discussed that chronic inflammatory masses may mimic soft tissue neoplasia, particularly when there are significant presentation delays. Ultrasound and CT are a valuable diagnostic tool in characterizing the lesion and extent of inflammatory process. These imaging modalities, however, are limited in further delineation of non-opacified stones from other liver lesions or tumors.
Intraoperative factors leading to gallstone spillage include tearing with fundal retraction, gallbladder decompression, or dissecting the gallbladder off the cystic plate.6 Additionally, when the gallbladder is removed from the port site, perforation can occur due to extraction under high pressures. Techniques to minimize iatrogenic gallbladder perforation include dissection in the correct plane between the liver and the gallbladder, minimizing diathermy injury, and use of blunt dissection in Calot’s dissection. If perforation has occurred, immediate intraoperative removal of as many spilled stones as possible is recommended; this may include using suction devices to retrieve spilled gallstones, collecting visible stones under laparoscopic vision, or closing the perforated hole using an endoclip or endoloop.11 The intraperitoneal space should be irrigated copiously to dilute the spilled bile contents and assist in visualization of retrieval of stones. Although retained gallstones can lead to significant postoperative morbidity, routine conversion to open technique to retrieve the stones is not recommended. Clear operative documentation of gallstone spillage in the operative record is recommended to prevent delays in diagnosis of hepatic pseudotumor in future presentations. Given that presentations of pseudotumors can be varied, retained gallstones warrants a high index of suspicion, and it is essential to review previous operative records.
Conclusion
The sequelae of retained gallstones are usually associated with an unexpected clinical presentation and can result in significant morbidity.4 The patient presented one year after an initial operation, having developed an inflammatory pseudotumor and subsequently requiring a hepatic resection, with potential significant complications. This report highlights the need for early prevention and recognition of spilled gallstones as well as the potential consequences of retained stones for the patient many years after the initial operation.
Lessons Learned
The consequences of spillage and unretrieved gallstones have varied presentations. The authors recommend that every effort be made to prevent stone spillage and complete retrieval of spilled gallstones at the time of the original operation as well as maintain clear operative documentation. In addition, surgeons must maintain a high index of suspicion given the varied clinical presentations.
Authors
Mwagiru DK; Pham H; Richardson AJ
Corresponding Author
Derek Mwagiru, MD, B BIOMED
Corner of Hawkesbury Road and Darcy Road
Westmead NSW 2145, Australia
Phone: +61400270962
E-mail: derek.mwagiru@gmail.com
Author Affiliation
Department of Surgery Westmead Hospital
Corner of Hawkesbury Road and Darcy Road Westmead NSW 2145, Australia
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Australian Government Department of Health. MBS Cholecystectomy Items. [Available from: http://www.medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp2017.
- Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006;(4):CD006231. Published 2006 Oct 18. doi:10.1002/14651858.CD006231
- Rammohan A, Srinivasan UP, Jeswanth S, Ravichandran P. Inflammatory pseudotumour secondary to spilled intra-abdominal gallstones. Int J Surg Case Rep. 2012;3(7):305-307. doi:10.1016/j.ijscr.2012.03.013
- Steerman PH, Steerman SN. Unretrieved gallstones presenting as a Streptococcus bovis liver abscess. JSLS. 2000;4(3):263-265.
- Arai T, Ikeno T, Miyamoto H. Spilled gallstones mimicking a liver tumor. Clin Gastroenterol Hepatol. 2012;10(11):A32. doi:10.1016/j.cgh.2012.06.026
- Bhati CS, Tamijmarane A, Bramhall SR. A tale of three spilled gall stones: one liver mass and two abscesses. Dig Surg. 2006;23(3):198-200. doi:10.1159/000094739
- Castellón-Pavón CJ, Morales-Artero S, Martínez-Pozuelo A, Valderrábano-González S. Complicaciones por cálculos y clips intraabdominales abandonados durante una colecistectomía laparoscópica [Complications due to spilled gallstones and surgical clips left in the abdomen during laparoscopic cholecystectomy]. Cir Esp. 2008;84(1):3-9. doi:10.1016/s0009-739x(08)70596-7
- Woodfield JC, Rodgers M, Windsor JA. Peritoneal gallstones following laparoscopic cholecystectomy: incidence, complications, and management. Surg Endosc. 2004;18(8):1200-1207. doi:10.1007/s00464-003-8260-4
- Casillas S, Kittur DS. Late abscess formation after spilled gallstones masquerading as a liver mass. Surg Endosc. 2003;17(5):833. doi:10.1007/s00464-002-4524-7
- Akhtar A, Bukhari MM, Tariq U, et al. Spilled Gallstones Silent for a Decade: A Case Report and Review of Literature. Cureus. 2018;10(7):e2921. Published 2018 Jul 5. doi:10.7759/cureus.2921
- Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg. 2007;193(1):73-78. doi:10.1016/j.amjsurg.2006.05.015