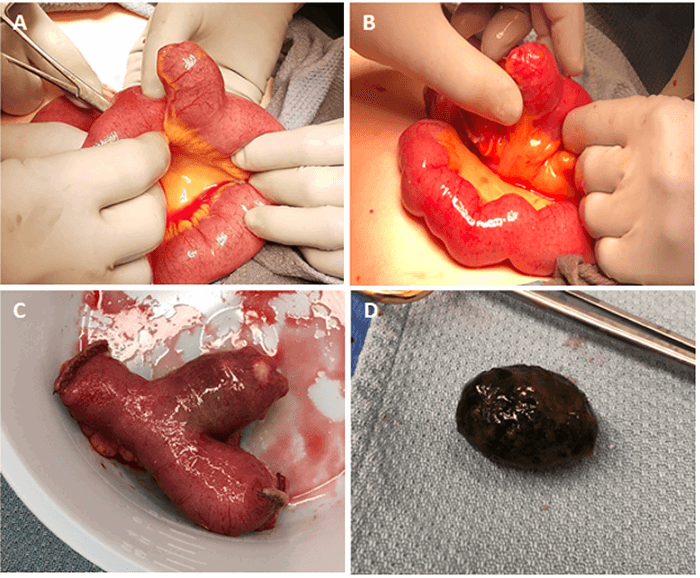
In these cases, we believe removal is advantageous because patients already require an enterolithotomy necessitating the opening of the small bowel. Removing the MD and gallstone can be combined into a single procedure by milking the gallstone to the MD, which can then be resected. This procedure is also the method described by Tan et al.8
There are three options for management of gallstone ileus: one-stage (enterolithotomy, cholecystectomy, and fistula repair), two-stage (enterolithotomy with delayed cholecystectomy and fistula repair one to six months later) 15–17 and enterolithotomy alone. Proponents of the one-stage approach cite reduced risk of gallstone ileus recurrence and gallbladder carcinoma as major reasons for concurrent cholecystectomy and fistula repair.18–21 There is an 8.2 percent risk of recurrence associated with 12 to 20 percent mortality when the fistula is not repaired.22 However, simple enterolithotomy has significantly lower mortality than one-stage procedures (11.7 percent to 16.9 percent). Some studies have found the risk of recurrence to be similar among all treatment modalities. 11,16,23 Despite these findings, a one-stage approach is still worth considering in healthy, hemodynamically stable patients to reduce visits to the OR.24–28 Our patient was a healthy 69-year-old woman who tolerated the bowel resection well, so the decision was made to address the gallbladder and duodenal fistula simultaneously in a one-stage procedure.
Finally, we propose that subtotal cholecystectomy is an effective method to mitigate some of the risks of one-stage procedures, particularly in patients with unclear anatomy. Subtotal cholecystectomy is a technique that involves excision or ablation of the gallbladder while leaving the most inferior portion intact, thereby avoiding the need for dissection or ligation of structures in Calot’s triangle. It has been increasingly used in patients with “difficult gallbladders” to avoid bile duct injuries.29–33 Compared to total cholecystectomies, subtotal cholecystectomies are associated with significantly fewer common bile duct injuries (0 percent to 3.3 percent) and fewer severe complications (0 percent to 7.9 percent) in complicated cholecystitis.34,35 In low-risk patients with gallstone ileus, this reduced complication rate is beneficial when deciding to undergo a one-stage procedure. There are already reports of subtotal cholecystectomies being utilized with success in one-stage operations for other types of gallbladder disease.36–38 In the future, it would be worthwhile to determine if the use of subtotal cholecystectomy in one-stage procedures could decrease morbidity and mortality to levels seen in simple enterolithotomy while retaining the advantages of decreased gallstone recurrence and need for re-operation.
Conclusion
Gallstone ileus is rare, especially in patients with no previous abdominal surgeries or medical comorbidities. Incidental MDs may be discovered during surgery, and management is controversial. In the setting of gallstone ileus, we recommend resection of incidental MD rather than simple enterolithotomy when feasible. Based on the literature, simple enterolithotomy is the current treatment of choice for gallstone ileus; however, a one-stage procedure can be considered for healthy, low-risk patients. Lastly, we describe the use of subtotal cholecystectomy in this case and propose that it can achieve similar outcomes and reduce complications associated with one-stage operations.
Lessons Learned
Although rare, gallstone ileus and Meckel’s diverticulum can be found, and it is important to have clearer guidelines on how to approach the management of MD and subsequent cholecystectomy. If the case is uncomplicated, a cholecystectomy with small bowel resection instead of an enterolithotomy alone can be considered.
Authors
Liem SSa; Liu Ca; Zheng Rb; Lundgren MPb; Aka AAb; Cohen Mb; Kohli Ab; Marks JAb
Author Affiliations
- Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA 19107
- Department of Surgery, Thomas Jefferson University, Philadelphia, PA 19107
Corresponding Author
Joshua A. Marks, MD
Thomas Jefferson University
Department of Surgery
1100 Walnut Street
Philadelphia, PA 19107
Phone: (215) 955-2165
E-mail: joshua.marks@jefferson.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Cullen, J J, and K A Kelly. “Current management of Meckel's diverticulum.” Advances in surgery vol. 29 (1996): 207-14.
- Moore, T C. “Omphalomesenteric duct malformations.” Seminars in pediatric surgery vol. 5,2 (1996): 116-23.
- Bani-Hani, Kamal E, and Nawaf J Shatnawi. “Meckel's diverticulum: comparison of incidental and symptomatic cases.” World journal of surgery vol. 28,9 (2004): 917-20. doi:10.1007/s00268-004-7512-3
- Sharma, Raj Kumar, and Vir Kumar Jain. “Emergency surgery for Meckel's diverticulum.” World journal of emergency surgery : WJES vol. 3 27. 13 Aug. 2008, doi:10.1186/1749-7922-3-27
- Ploneda-Valencia, C F et al. “Gallstone ileus: An overview of the literature.” “El íleo biliar: una revisión de la literatura médica.” Revista de gastroenterologia de Mexico vol. 82,3 (2017): 248-254. doi:10.1016/j.rgmx.2016.07.006
- Artioli, Giulia et al. “Gallstone ileus: literature review.” Acta bio-medica : Atenei Parmensis vol. 87 Suppl 3 40-4. 28 Jul. 2016
- Lamba, Harveen K et al. “Gallstone ileus associated with impaction at Meckel's diverticulum: Case report and literature review.” World journal of gastrointestinal surgery vol. 8,11 (2016): 755-760. doi:10.4240/wjgs.v8.i11.755
- Tan, Hwee Leong et al. “An Unusual Case of Small Bowel Obstruction in an Elderly Woman.” Gastroenterology vol. 150,7 (2016): e3-e4. doi:10.1053/j.gastro.2016.02.008
- Maclean, William, and Karoly Szentpáli. “Large gallstone impaction at a Meckel's diverticulum causing perforation and localized peritonitis: report of a case.” Journal of surgical case reports vol. 2013,12 rjt097. 4 Dec. 2013, doi:10.1093/jscr/rjt097
- Nakamoto, Y et al. “Gallstone ileus with impaction at the neck of a Meckel's diverticulum.” The British journal of radiology vol. 71,852 (1998): 1320-2. doi:10.1259/bjr.71.852.10319010
- Reisner, R M, and J R Cohen. “Gallstone ileus: a review of 1001 reported cases.” The American surgeon vol. 60,6 (1994): 441-6.
- Peoples, J B et al. “Incidental Meckel's diverticulectomy in adults.” Surgery vol. 118,4 (1995): 649-52. doi:10.1016/s0039-6060(05)80031-5
- Zani, Augusto et al. “Incidentally detected Meckel diverticulum: to resect or not to resect?.” Annals of surgery vol. 247,2 (2008): 276-81. doi:10.1097/SLA.0b013e31815aaaf8
- Cullen, J J et al. “Surgical management of Meckel's diverticulum. An epidemiologic, population-based study.” Annals of surgery vol. 220,4 (1994): 564-8; discussion 568-9. doi:10.1097/00000658-199410000-00014
- Inukai, Koichi et al. “Laparoscopic two-stage procedure for gallstone ileus.” Journal of minimal access surgery, vol. 15,2 164–166. 27 Jun. 2018, doi:10.4103/jmas.JMAS_88_18
- Salazar-Jiménez, Marcos I et al. “Íleo biliar, revisión del manejo quirúrgico” [Gallstone ileus, surgical management review]. Cirugia y cirujanos vol. 86,2 (2018): 182-186. doi:10.24875/CIRU.M18000032
- Ploneda-Valencia, C F et al. “Gallstone ileus: An overview of the literature.” “El íleo biliar: una revisión de la literatura médica.” Revista de gastroenterologia de Mexico vol. 82,3 (2017): 248-254. doi:10.1016/j.rgmx.2016.07.006
- Berliner, S D, and L C Burson. “One-Stage Repair for Cholecyst-Duodenal Fistula and Gallstone Ileus.” Archives of surgery (Chicago, Ill. : 1960) vol. 90 (1965): 313-6. doi:10.1001/archsurg.1965.01320080137028
- Nuño-Guzmán, Carlos M et al. “Gallstone ileus: One-stage surgery in a patient with intermittent obstruction.” World journal of gastrointestinal surgery vol. 2,5 (2010): 172-6. doi:10.4240/wjgs.v2.i5.172
- Williams, Nicholas E et al. “Disease spectrum and use of cholecystolithotomy in gallstone ileus transection.” Hepatobiliary & pancreatic diseases international : HBPD INT vol. 11,5 (2012): 553-7. doi:10.1016/s1499-3872(12)60224-0
- Bossart, P A et al. “Carcinoma of the gallbladder. A report of seventy-six cases.” American journal of surgery vol. 103 (1962): 366-9. doi:10.1016/0002-9610(62)90227-1
- Doogue, M P et al. “Recurrent gallstone ileus: underestimated.” The Australian and New Zealand journal of surgery vol. 68,11 (1998): 755-6. doi:10.1111/j.1445-2197.1998.tb04669.x
- Halabi, Wissam J et al. “Surgery for gallstone ileus: a nationwide comparison of trends and outcomes.” Annals of surgery vol. 259,2 (2014): 329-35. doi:10.1097/SLA.0b013e31827eefed
- Clavien, P A et al. “Gallstone ileus.” The British journal of surgery vol. 77,7 (1990): 737-42. doi:10.1002/bjs.1800770707
- Pavlidis, Theodoros E et al. “Management of gallstone ileus.” Journal of hepato-biliary-pancreatic surgery vol. 10,4 (2003): 299-302. doi:10.1007/s00534-002-0806-7
- Mallipeddi, Mohan K et al. “Gallstone ileus: revisiting surgical outcomes using National Surgical Quality Improvement Program data.” The Journal of surgical research vol. 184,1 (2013): 84-8. doi:10.1016/j.jss.2013.05.027
- Rodríguez-Sanjuán, J C et al. “Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus.” The British journal of surgery vol. 84,5 (1997): 634-7.
- Riaz, N et al. “Gallstone ileus: retrospective review of a single centre's experience using two surgical procedures.” Singapore medical journal vol. 49,8 (2008): 624-6.
- Elshaer, Mohamed et al. “Subtotal cholecystectomy for "difficult gallbladders": systematic review and meta-analysis.” JAMA surgery vol. 150,2 (2015): 159-68. doi:10.1001/jamasurg.2014.1219
- Shingu, Yuji et al. “Laparoscopic subtotal cholecystectomy for severe cholecystitis.” Surgical endoscopy vol. 30,2 (2016): 526-531. doi:10.1007/s00464-015-4235-5
- Harilingam, Mohan Raj et al. “Laparoscopic modified subtotal cholecystectomy for difficult gall bladders: A single-centre experience.” Journal of minimal access surgery vol. 12,4 (2016): 325-9. doi:10.4103/0972-9941.181323
- Jara, Génesis et al. “Laparoscopic subtotal cholecystectomy: a surgical alternative to reduce complications in complex cases.” “Colecistectomía laparoscópica subtotal como alternativa quirúrgica segura en casos complejos.” Cirugia espanola vol. 95,8 (2017): 465-470. doi:10.1016/j.ciresp.2017.07.013
- Abdelrahim, W E et al. “Subtotal laparoscopic cholecystectomy influences the rate of conversion in patients with difficult laparoscopic cholecystectomy: Case series.” Annals of medicine and surgery (2012) vol. 19 19-22. 25 May. 2017, doi:10.1016/j.amsu.2017.04.018
- Strasberg, Steven M et al. “Subtotal Cholecystectomy-"Fenestrating" vs "Reconstituting" Subtypes and the Prevention of Bile Duct Injury: Definition of the Optimal Procedure in Difficult Operative Conditions.” Journal of the American College of Surgeons vol. 222,1 (2016): 89-96. doi:10.1016/j.jamcollsurg.2015.09.019
- Kaplan, Daniel et al. “Subtotal cholecystectomy and open total cholecystectomy: alternatives in complicated cholecystitis.” The American surgeon vol. 80,10 (2014): 953-5.
- Yang, Dong et al. “Laparoscopic treatment of an upper gastrointestinal obstruction due to Bouveret's syndrome.” World journal of gastroenterology vol. 19,40 (2013): 6943-6. doi:10.3748/wjg.v19.i40.6943
- Glaysher, Michael A et al. “A rare cause of upper gastrointestinal haemorrhage: Ruptured cystic artery pseudoaneurysm with concurrent cholecystojejunal fistula.” International journal of surgery case reports vol. 5,1 (2014): 1-4. doi:10.1016/j.ijscr.2013.11.005
- Periselneris, N, and J J Bong. “Choledocho-duodenal fistula encountered during emergency laparotomy for upper gastro-intestinal haemorrhage: what should be the surgical strategy?.” La Clinica terapeutica vol. 162,6 (2011): 547-8.