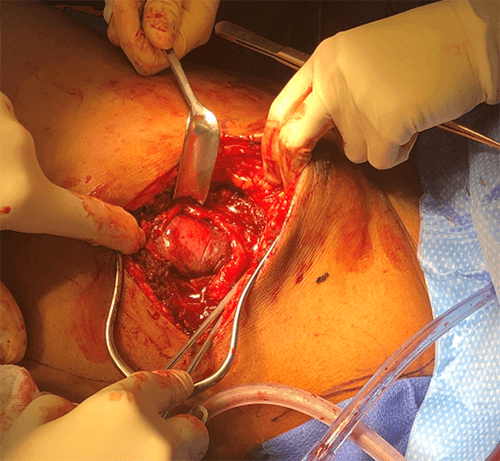
A 32-French apical chest tube was placed under direct visualization. The defect between the ribs was closed with an intercostal muscle flap and pericostal sutures. Given the proximity to the mediastinum, fixation of a mesh was not possible. An intercostal nerve block was performed with liposomal bupivacaine and the patient was taken to the trauma intensive care unit postoperatively. He was extubated shortly following surgery with a vital capacity of 1.5 liters.
The patient had an uneventful hospital course and was discharged on postoperative day five. He has been seen twice in our outpatient office, most recently two months post-operatively. His pain remains under control and has incurred no respiratory complications.
Discussion
Pulmonary hernias are uncommon. Only approximately 300 cases were reported in the literature1 since Roland first described herniation of the lung in 1499.2 Chest wall hernias were later classified by Morel-Lavalée in 1847.3 They are described by anatomic or etiologic classification. From an anatomic perspective, herniation may occur in the cervical, intercostal, or diaphragmatic regions. The etiological group is further subdivided into congenital (20 percent) or acquired (80 percent).4 Most of the acquired etiologies are traumatic (52 percent), but they may also occur spontaneously (30 percent) or due to underlying lung pathology (18 percent).5 Chest wall hernias occur most frequently in the anterior chest, near the sternum. This is due to the lack of muscular support from the latissimus, rhomboid, and trapezius muscles.6
Prospective data on the most effective surgical management of lung herniation is lacking. Rigid prostheses provide chest wall stability and potentially decrease respiratory complication; however, they may be associated with more wound complications. Generally, posterior and apical defects do not require chest wall reconstruction, given the natural structure of the sternum, scapula, and clavicle. Defects closer to ribs five and six may require synthetic mesh to bridge the gap. Many large anterior and lateral defects are associated with paradoxical chest wall motion and need rigid reconstruction with plates.7
In 2002, Weissberg et al., published one of the largest single-center case series. They looked at eight patients over 17 years old who had lung herniation. Three cases were postoperative hernias, one was due to chronic cough, and four were congenital in origin. Three cases were managed nonoperatively as they had minimal symptoms. Four cases were managed with pericostal fixation, and one large defect was repaired with a Marlex mesh patch. There were no recurrences.8 Identifying which patients to repair surgically and which to observe is another area in question concerning chest wall defects and lung herniation. Small, asymptomatic hernias may heal spontaneously or remain occult.9 Hernias that are larger, or associated with flail chest, benefit from rib fixation, closure of the chest wall defect or both.10
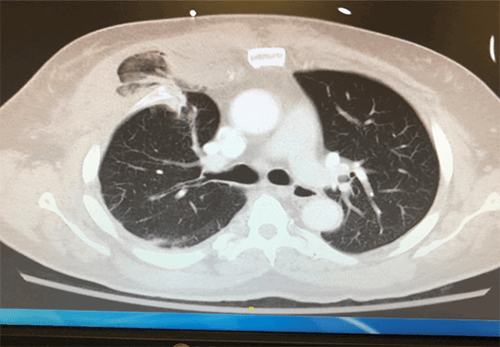
Another large case series published in 2018 by Kuckelman et al. examined 24 patients over 32 years. They developed an operative grade for traumatic rib cage hernias (TRCH) to standardize operative care. By their grading scheme, the patient described above would have classified as grade 2 TRCH, he had multiple displaced rib fractures and an intercostal muscle defect of greater than two centimeters with partial organ herniation. Based on this, the repair recommendations made by Kuckelman and coauthors are akin to what was performed with the current patient: rib plating with primary repair of the chest wall defect. Although that study involves a small sample size, given the rare nature of TRCH, they describe a novel approach to this complex surgical condition.11
In our case study, the defect was small and easily covered by an intercostal muscle flap. The proximity of the high, antero-medial chest wall disruption was too close to major mediastinal structures to secure a mesh patch safely. The patient did well postoperatively from respiratory, pain, and functional standpoints.
Conclusion
Lung herniation is an uncommon condition. Management strategies are non-standardized and patient-specific. We describe the case of a traumatic pulmonary hernia due to rib fractures following a motor vehicle collision. This patient was treated with hernia reduction, rib fixation with an intercostal flap to bridge the defect, and local nerve blockade. He had minimal postoperative pain and an uneventful hospital course. This case demonstrates the importance of tailoring the treatment of lung herniation to patient symptomatology and the reduction of morbidity.
Lessons Learned
Traumatic pulmonary herniation is rare and has no standard management guidelines. Treatment planning is based on patient symptomatology, size of the defect, location of the defect, and the severity of any associated rib fractures. Operative strategies should aim to reduce pain and improve respiratory status with as little morbidity as possible.
Authors
Teichman ALa; Perea LLb; Chovanes JJc
Author Affiliations
- Robert Wood Johnson University Hospital, Department of Surgery-Division of Acute Care Surgery,
New Brunswick, NJ 08901
- Lancaster General Health, Department of Surgery-Division of Trauma and Acute Care Surgery, Lancaster, PA 17602
- Cooper University Hospital, Department of Surgery-Division of Trauma and Acute Care Surgery,
Camden, NJ 08103
Corresponding Author
Amanda L. Teichman, MD
Robert Wood Johnson University Hospital
Department of Surgery, Division of Acute Care Surgery
125 Paterson Street, Ste. 6300
New Brunswick, NJ 08901
Phone: (908) 216-6053
E-mail: ateich13@rwjms.rutgers.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Fackeldey V, Junge K, Hinck D, et al. Repair of intercostal pulmonary herniation. Hernia. 2003;7(4):215-217. doi:10.1007/s10029-003-0135-z
- Roland. De Pulmonis sanaripot. De Chavliae G. 1499;XXV(III):144
- Morel-Lavallée A. Hernies Du poumon. Bull Soc Chir Paris 1845–1847;1:75–195.
- Tack D, Wattiez A, Schtickzelle JC, Delcour C. Spontaneous lung herniation after a single cough. Eur Radiol. 2000;10(3):500-502. doi:10.1007/s003300050084
- Akkas Y, Peri NG, Kocer B, Kaplan T. Repair of lung herniation with titanium prosthetic ribs and Prolene mesh. Asian Cardiovasc Thorac Ann. 2016;24(3):280-282. doi:10.1177/0218492315619509
- Sulaiman A, Cottin V, De Souza Neto EP, et al. Cough-induced intercostal lung herniation requiring surgery: Report of a case. Surg Today. 2006;36(11):978-980. doi:10.1007/s00595-006-3284-8
- Thomas PA, Brouchet L. Prosthetic reconstruction of the chest wall. Thorac Surg Clin. 2010;20(4):551-558. doi:10.1016/j.thorsurg.2010.06.006
- Weissberg D, Refaely Y. Hernia of the lung. Ann Thorac Surg. 2002;74(6):1963-1966. doi:10.1016/s0003-4975(02)04077-8
- Arslanian A, Oliaro A, Donati G, Filosso PL. Posttraumatic pulmonary hernia. J Thorac Cardiovasc Surg. 2001;122(3):619-621. doi:10.1067/mtc.2001.114630
- Slobogean GP, MacPherson CA, Sun T, Pelletier ME, Hameed SM. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg. 2013;216(2):302-11.e1. doi:10.1016/j.jamcollsurg.2012.10.010
- Kuckelman J, Karmy-Jones R, Windell E, et al. Traumatic thoracic rib cage hernias: Operative management and proposal for a new anatomic-based grading system. Am J Surg. 2018;215(5):794-800. doi:10.1016/j.amjsurg.2017.12.013