
Diagnostic and Therapeutic Challenges in a Rare Case of Multifocal Primary Ectopic Breast Carcinoma of the Chest Wall
Multifocal primary ectopic breast cancer is very rare and difficult to diagnose using conventional methods of screening
July 8, 2021
Abstract
Background
Ectopic breast tissue can be found anywhere along the embryonic mammary ridges, most commonly in the axilla and vulva. Because ectopic tissue is under the same hormonal control as native breast tissue, it is also at risk for malignant transformation. Due to their rarity, however, there is low clinical suspicion and a lack of screening for neoplasms in these locations. As a result, ectopic breast carcinoma (EBC) is often advanced at the time of diagnosis and, therefore, more difficult to treat than carcinomas in the native breast.
Summary
A 59-year-old female presented with an enlarging mass just beneath her right inframammary fold. An ultrasound-guided biopsy revealed a hormone receptor (HR)-negative and HER2-positive invasive ductal carcinoma (IDC). A breast MRI was performed, and a second ectopic area of enhancement was seen, which was subsequently biopsied and found to be IDC with the same receptor status. No lesions were noted in either native breast. PET-CT did not reveal any foci of metastatic disease, and preoperative lymphoscintigraphy failed to identify sentinel lymph nodes. She went on to have a full excision of the identifiable ectopic breast tissue following Tc-99 colloid and blue dye injection, which again failed to localize sentinel lymph nodes. The specimen consisted of two foci of high-grade IDC (2.1 and 1 cm, respectively) on analysis. The patient underwent adjuvant chemotherapy and radiation, is undergoing surveillance with annual mammography and MRI, and has no evidence of recurrent disease three years later.
Conclusion
Multifocal primary ectopic breast cancer is very rare and difficult to diagnose using conventional methods of screening. We present a case of a patient with HR-negative and HER2-positive multifocal ectopic IDC. The patient had upfront surgery due to a concern for an inability to localize these areas after neoadjuvant therapy. A failure to map sentinel nodes precluded complete staging in this case, so the patient was treated with definitive adjuvant therapies. The consensus is that EBC should be treated as if it arose in the native breast. Despite guidelines for treating native breast cancer, the management of EBC is confounded by anatomic and biologic variability, which makes screening, staging, and treatment more challenging.
Key Words
ectopic; multifocal; breast cancer; adjuvant therapy; lymphoscintigraphy
Case Description
Mammary tissue arises from epithelial cells that proliferate along bilateral ridges between the fetal axilla and inguinal region, the so-called milk lines or mammary crests, as early as 4–6 weeks of gestation.1 Except for the two mammary buds, the remainder of this tissue typically regresses by the end of the first trimester. The failure of this tissue to regress results in ectopic breast tissue (EBT), which can be present anywhere along the mammary ridge. Ultimately varying degrees of phenotypic features can be seen with EBT from clinically undetectable to the presence of a nipple and/or areola. EBT, the true incidence of which is unknown, is rare but undergoes the same physiologic changes throughout life as native breast tissue, including both benign and malignant pathologic changes. Ectopic breast cancer (EBC) is a rare entity that most frequently arises in the axilla2 and poses a diagnostic and therapeutic dilemma. We present a unique case of multifocal, HER2-positive invasive ductal carcinoma in ectopic breast tissue of the inferior chest wall.
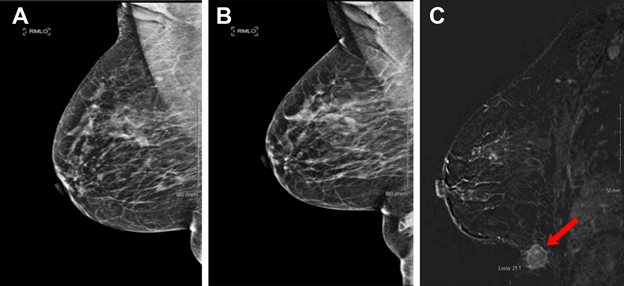
A 59-year-old G3P3 post-menopausal female with a past medical history of hypertension presented to her primary care physician for routine checkup and noted a lump inferior to her right inframammary fold. She described the lump as presenting for longer than one year but had been progressively enlarging. She was referred for an ultrasound of the area which demonstrated a 25 mm x 16 mm x 18 mm lobulated mass. Mammography performed at the same time with an attempt to image the area of concern showed a density corresponding to the palpable area of concern that was not appreciated on previous examinations since it was not in the field of view (Figure 1A and Figure 1B). A core needle biopsy of the mass was performed under ultrasound guidance, and pathologic analysis showed invasive ductal (IDC), which was estrogen receptor (ER)-negative and progesterone receptor (PR)-negative, and HER2-positive. Given other benign findings on mammography, a breast MRI was performed (Figure 1C), which demonstrated a second, 8 mm spiculated nodule inferior and lateral to the previously biopsied mass along the abdominal wall. This mass also underwent ultrasound-guided core needle biopsy, which demonstrated ER-negative, PR-negative, and HER2-positive IDC.
Figure 1. Mammogram six months before A) and after B) patient presented with a complaint of an enlarging chest wall mass with a skin marker (triangle) placed over the palpable tumor; the mass is best seen on MRI (C, arrow)
At this point, the discussion with radiology and medical oncology centered around several dilemmas. First, since the patient had a 2 cm HER2-positive breast cancer, she met the criteria for neoadjuvant anti-HER2 therapy. However, since the second focus of IDC was not able to be seen on a mammogram, preoperative localization of the lesion would be especially challenging if she had a complete clinical response to neoadjuvant therapy. Therefore, the decision was made to pursue surgery upfront. The second dilemma was around the assessment of regional and distant metastatic disease. While the likelihood of distant metastasis was low, the patient did undergo PET-CT, which ultimately did not reveal evidence of metastasis. Related to regional lymph nodes, it was not known to which nodal basin the tumors drained, with the axilla and the groin both being possible, so the patient underwent lymphoscintigraphy. This study, unfortunately, did not localize to any nodal basin, so the decision was made to attempt sentinel lymph node injection at the time of surgery.
The day following lymphoscintigraphy, the patient was taken to the operating room for excision. Ultrasound-guided wire localization of the nonpalpable posterior mass was performed, and blue dye was injected into the palpable portion of the anterior mass (Figure 2A). The entire volume of ectopic breast tissue was excised (Figure 2B). Despite excellent gamma activity at the injection site, there was no gamma activity in the ipsilateral axilla nor groin. Surgical exploration of the axilla yielded normal lymph nodes, but none that were blue or had taken up Tc-99 colloid, and there were no blue lymphatics. The decision was made not to perform any lymphadenectomy. Final pathology was consistent with high-grade IDC in the background of ectopic breast tissue (Figure 3). The patient ultimately underwent adjuvant chemotherapy with Taxotere, carboplatin, and trastuzumab, along with adjuvant radiation therapy. Radiation fields included only the accessory breast tissue, which was initially treated to 5,000 cGy with a subsequent 1,600 cGy boost. The ipsilateral breast was not treated. She continues with annual mammography and clinical examination and has no evidence of recurrent disease after three years.
Figure 2. A) Preoperative wire localization of the nonpalpable (#2) posterior lesion; and (B) postoperative result after the entire volume of ectopic breast tissue was excised
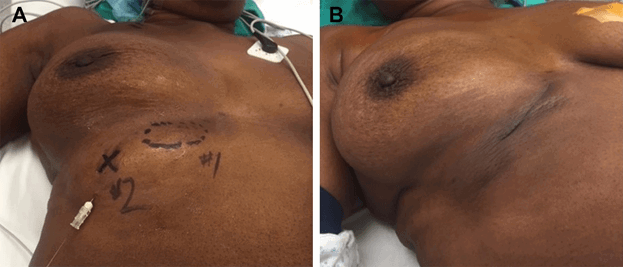
Figure 3. High grade invasive ductal carcinoma (right) invading benign mammary ducts of ectopic breast tissue in the final pathologic specimen

Discussion
Ectopic breast cancer presents several diagnostic and therapeutic challenges. EBC is more challenging to diagnose than breast cancer in the native breast mostly due to lack of screening in the locations where it typically presents. The literature contains many case reports and several reviews of EBC, most of which indicate the most common location for EBC is the axilla,2–4 which is typically part of the clinical breast examination. Other locations described include in accessory breast tissue with visible nipple,5 several cases in the vulva,6–9 and even one case of a male patient with EBC in the perineum.10 Due to the ectopic location of these carcinomas, there is often a delay in diagnosis, which Visconti et al. cite as up to 40.5 months.11 This delay in diagnosis corresponds with the fact that many EBCs are locally invasive or metastatic at the time of diagnosis and require more radical treatment than most cancers diagnosed in the native breast.3,5,12,13 Once a mass is recognized, radiographic evaluation more than often does not clarify the diagnosis, prompting complete pathologic workup.14 The diagnosis of EBC may further be complicated if benign breast parenchyma is not identified within a biopsy specimen.2
Once a diagnosis of EBC has been made, most reports advocate for treatment dictated by conventional algorithms used in treating native breast cancer.15 The variability of the location of EBC, however, does require individualization of these treatment algorithms. As in native breast cancer, preoperatively assessing for distant metastatic disease is an important step in patients who have advanced tumors at the time of presentation. Unlike in native breast cancer, the nodal basin to which the EBC drains may be unknown, so clinical examination of the axilla and groin is important. Preoperative lymphoscintigraphy may be helpful in assessing lymphatic draining patterns and directing intraoperative nodal assessment but may also be non-diagnostic, as in the case presented. Sentinel lymph node mapping, as described in the treatment of melanoma, which arises in disparate locations, can be used as a model.16,17 Some reports of EBC describe performing axillary sentinel lymphadenectomy18 in congruence with the treatment of native breast cancer, while Nihon et al. describe a complete axillary lymph node dissection for an axillary EBC.19 There are no prospective data to suggest the benefit of complete axillary lymph node dissection in EBC in the absence of locally invasive primary axillary EBC or >2 positive axillary sentinel lymph nodes as described in the ACOSOG Z0011 paradigm.20 Regarding the primary tumor, wide local excision of the EBC is the most commonly reported approach, and the historical practice of ipsilateral mastectomy for axillary or chest wall EBC is no longer advised.5,7,15
Our case is unique because there is only one other report in the literature of a multifocal EBC,4 and most cases do not demonstrate a dilemma in whether to proceed with upfront surgery or neoadjuvant systemic therapy. Our patient is also unique in that complete staging was not possible due to failure of lymph node mapping. In addition, unlike the majority of cases in the literature that are hormone receptor-positive, her tumor was hormone receptor-negative and HER2 positive.5,15 As a result, she was treated with adjuvant chemotherapy, anti-HER2 therapy, and radiation but is not undergoing ongoing anti-estrogen therapy. Despite these challenges, the patient is well without evidence of disease three years after her surgical treatment.
Conclusion
While ectopic breast tissue is fairly common, ectopic breast cancer is rare and unique due to its anatomic and biologic variability and its tendency toward remaining occult until it is advanced. We present a case of multifocal ectopic breast cancer and detail our attempts to identify sentinel lymph nodes and stage the tumors. Our diagnostic and surgical findings informed our adjuvant treatment strategies. This highlights the need to tailor diagnostic studies and therapeutic modalities to a patient’s specific ectopic breast cancer.
Lessons Learned
Ectopic breast cancer is both rare and unique due to its anatomic and biologic variability. While treatment should be based on algorithms for breast cancer of the native breast, diagnostic studies and therapeutic modalities may be tailored to a patient’s specific disease.
Authors
Williams AD; Salim AN; Ciocca RM
Author Affiliation
Lankenau Medical Center, Department of Surgery, Wynnewood, PA 19096
Corresponding Author
Robin Ciocca, DO
Lankenau Medical Center, Medical Science Building
100 E. Lancaster Avenue, Ste. 275
Wynnewood, PA 19096
E-mail: cioccar@mlhs.org
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Javed A, Lteif A. Development of the human breast. Semin Plast Surg. 2013;27(1):5-12. doi:10.1055/s-0033-1343989
- Gutermuth J, Audring H, Voit C, Haas N. Primary carcinoma of ectopic axillary breast tissue. J Eur Acad Dermatol Venereol. 2006;20(2):217-221. doi:10.1111/j.1468-3083.2005.01362.x
- Kahraman-Cetintas S, Turan-Ozdemir S, Topal U, et al. Carcinoma originating from aberrant breast tissue. A case report and review of the literature. Tumori. 2008;94(3):440-443.
- Corsi F, Sartani A, Rizzi A, et al. Primary carcinoma of ectopic breast tissue. Clin Breast Cancer. 2008;8(2):189-191. doi:10.3816/CBC.2008.n.021
- Hallam S, Aggarwal A, Predolac D, Cunnick G, Ashford R. Primary ectopic breast carcinoma in a supernumerary breast arising in the anterior chest wall: a case report and review of the literature. J Surg Case Rep. 2013;2013(12):rjt107. Published 2013 Dec 16. doi:10.1093/jscr/rjt107
- Lopes G, DeCesare T, Ghurani G, et al. Primary ectopic breast cancer presenting as a vulvar mass. Clin Breast Cancer. 2006;7(3):278-279. doi:10.3816/CBC.2006.n.041
- McMaster J, Dua A, Dowdy SC. Primary breast adenocarcinoma in ectopic breast tissue in the vulva. Case Rep Obstet Gynecol. 2013;2013:721696. doi:10.1155/2013/721696
- Chung-Park M, Zheng Liu C, Giampoli EJ, Emery JD, Shalodi A. Mucinous adenocarcinoma of ectopic breast tissue of the vulva. Arch Pathol Lab Med. 2002;126(10):1216-1218. doi:10.5858/2002-126-1216-MAOEBT
- Ahmed M, Aurangzeb, Pervez A, Kamal Z, Younas A. Primary carcinoma of ectopic breast tissue in axilla. J Coll Physicians Surg Pak. 2012;22(11):726-727.
- Eom HJ, Ko BS, Song IH, Gong G, Kim HH. Ectopic male breast cancer in the perineum: a case report. J Breast Cancer. 2017;20(4):404-407. doi:10.4048/jbc.2017.20.4.404
- Visconti G, Eltahir Y, Van Ginkel RJ, Bart J, Werker PM. Approach and management of primary ectopic breast carcinoma in the axilla: where are we? A comprehensive historical literature review. J Plast Reconstr Aesthet Surg. 2011;64(1):e1-e11. doi:10.1016/j.bjps.2010.08.015
- Caceres M, Shih J, Eckert M, Gardner R. Metaplastic carcinoma in an ectopic breast. South Med J. 2002;95(4):462-466.
- Kayılıoğlu SI, Akyol C, Esen E, et al. Gastric metastasis of ectopic breast cancer mimicking axillary metastasis of primary gastric cancer. Case Rep Gastrointest Med. 2014;2014:232165. doi:10.1155/2014/232165
- Oudsema R, Simpson W, Szabo J, Margolies LR. The mammary ridge-A case report of multiple ectopic breast masses. Clin Imaging. 2017;45:34-36. doi:10.1016/j.clinimag.2017.05.012
- Roorda AK, Hansen JP, Rider JA, Huang S, Rider DL. Ectopic breast cancer: special treatment considerations in the postmenopausal patient. Breast J. 2002;8(5):286-289. doi:10.1046/j.1524-4741.2002.08507.x
- Dias Moreira R, Altino de Almeida S, Maliska Guimarães CM, Resende JF, Gutfilen B, Barbosa da Fonseca LM. Sentinel node identification by scintigraphic methods in cutaneous melanoma. J Exp Clin Cancer Res. 2005;24(2):181-185.
- Baldwin BT, Cherpelis BS, Sondak V, Fenske NA. Sentinel lymph node biopsy in melanoma: Facts and controversies. Clin Dermatol. 2010;28(3):319-323. doi:10.1016/j.clindermatol.2009.06.016
- Alavifard R, Kadkhodayan S, Homaee Shandiz F, Dabbagh VR, Sadeghi R. Is sentinel node mapping possible in surgically removed ectopic axillary breast cancer? A case report. Nucl Med Rev Cent East Eur. 2016;19(B):29-30. doi:10.5603/NMR.2016.0036
- Nihon-Yanagi Y, Ueda T, Kameda N, Okazumi S. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011;20(1):35-42. doi:10.1016/j.suronc.2009.09.005
- Giuliano AE, Ballman KV, McCall L, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318(10):918-926. doi:10.1001/jama.2017.11470