Abstract
Background
Damage control laparotomy is a strategy used when dealing with intra-abdominal catastrophe. The open abdomen, one of the elements of this strategy, decreases the incidence of abdominal compartment syndrome and allows for serial second-look laparotomies to stabilize the intra-abdominal process prior to definitive abdominal wall closure. While direct closure of fascia is ideal, this is sometimes not possible, and other methods of definitive abdominal wall closure must instead be explored.
Summary
This case report details the clinical presentation and treatment of a 52-year-old male with mixed ischemic and non-ischemic cardiomyopathy with an ejection fraction of 10 percent and dual-chamber implantable cardioverter-defibrillator (ICD) who deteriorated into ventricular tachycardia (VT) storm and biventricular cardiogenic shock with multiple organ system failure requiring VA-ECMO (veno-arterial extracorporeal membrane oxygenation). He was transitioned to bilateral CentriMag® devices but developed a large, right retroperitoneal hematoma requiring decompressive laparotomy. Direct fascial closure was not possible, and thus his abdomen was closed with an inlay bridge biologic mesh, and a wound vacuum was placed over the mesh. Due to the large skin and subcutaneous tissue gap between skin flaps not amenable to primary closure, two DermaClose® systems were put into the skin in combination with wound vacuum therapy. The DermaClose® was originally designed for the closure of small extremity wounds. The DermaClose® system allowed for abdominal wall skin flap primary closure.
Conclusion
This is the first case report detailing our novel modification of the DermaClose® system in combination with wound vacuum therapy on the abdominal wall in a critically ill cardiac patient with an open abdomen and a large skin flap gap. With our modification, our patient was able to undergo successful abdominal wall closure and heart transplantation.
Key Words
abdominal compartment syndrome; open abdomen
Case Description
Damage control laparotomy is a commonly used strategy when dealing with intra-abdominal catastrophe. The open abdomen is one of the elements of this strategy. The open abdomen with temporary abdominal wall closure is indicated in the presence of the "triad of death" (coagulopathy, acidosis, and hypothermia) and situations associated with an increased risk of postoperative abdominal compartment syndrome (ACS). In conditions such as these, immediate closure of the abdomen may further compromise the patient's physiology.
Abdominal compartment syndrome is defined as an increase in intra-abdominal pressure leading to decreased cardiac preload, and increased intra-thoracic pressure resulting in cardiovascular collapse, acute respiratory failure, and acute kidney injury. The causes of ACS are multiple and include intra-abdominal trauma, ruptured abdominal aortic aneurysm, retroperitoneal hemorrhage, acute pancreatitis, burns, excessive fluid resuscitation, and sepsis, among others.1 Once the abdomen has been opened, various methods have been described to protect the abdominal contents and preserve the abdominal domain. These methods include different modifications of temporary abdominal wall dressings with negative pressure wound therapy (wound vacuum), Wittmann patch with transabdominal wall traction (TAWT), and other systems to preserve the abdominal domain.2,3
Definitive abdominal wall closure should not be delayed, however, as early closure of the abdomen has been shown to improve survival in these patients significantly.4,5 Once the patient's intra-abdominal conditions requiring an open abdomen are controlled and overall physiology normalized, final abdominal closure should be attempted.5 Direct closure of the fascia and skin is ideal. Still, this is not feasible in many cases due to loss of abdominal domain, extensive peritoneal adhesions, and excessive edema of intraabdominal organs and retroperitoneal structures. Therefore, other permanent abdominal wall closure techniques may be used alone or in combination: skin grafting over the granulated open abdomen, mesh-augmented closure with either synthetic or biologic products as an inlay or underlay, and component separations.6–8 Of note, pedicle or free flap abdominal wall reconstruction should be mentioned as a last resort in the reconstructive ladder that should only be undertaken as part of a multidisciplinary team with plastic surgery involvement.8
This case report describes a novel method of definitive abdominal wall closure in a patient with both a right ventricular assist device (RVAD) and left ventricular assist device (LVAD) who developed ACS secondary to a retroperitoneal hematoma necessitating decompressive laparotomy.
The patient is a 52-year-old male with a past medical history of mixed ischemic and non-ischemic cardiomyopathy with an ejection fraction of 10 percent and dual-chamber implantable cardioverter-defibrillator (ICD). He was transferred to our institution for evaluation of advanced cardiac support therapies (ventricular assist devices and orthotopic heart transplant) after deteriorating into ventricular tachycardia (VT) storm. Aggressive medical therapy for VT was unsuccessful, and he continued to deteriorate with VT storm and associated biventricular cardiogenic shock with multiple organ system failure (respiratory failure, shock liver, and hepatic encephalopathy) requiring peripheral VA-ECMO (veno-arterial extrcorporeal membrane oxygenation). This was achieved through 25 French right femoral vein cannula, 19 French right femoral arterial cannula, and 7 French antegrade catheter in superficial femoral artery for perfusion of the right lower extremity. He was transitioned eight days later to central cannulation with bilateral CentriMag® devices, and peripheral VA-ECMO cannulae were removed. Ten days after removal of ECMO cannulae, the patient developed an acute drop in his hematocrit resulting in an emergent computed tomography (CT) of his abdomen and pelvis. This showed a large right retroperitoneal hematoma without associated arterial pseudoaneurysm but presumed secondary to ECMO cannulation and systemic anticoagulation management. The patient developed the clinical picture of abdominal compartment syndrome and was emergently taken to the operating room for decompressive laparotomy with temporary abdominal wall closure. During exploration, the retroperitoneal hematoma was visualized but not evacuated as it was stable in size during the operation.
After the surgery, the patient was taken back to the cardiothoracic ICU for resuscitation. Forty-eight hours later, after extensive diuresis, the patient was taken to the operative room. The definitive abdominal fascia closure was impossible, given his tenuous cardiac function and excessive third spacing. Instead, we elected to place a Wittman patch with a transabdominal wall traction system and negative pressure dressing with plans for every other day tightening of the Wittmann patch. This is our standard approach to managing the difficult open abdomen. During the next 18 days, he returned to the operating room for abdominal washouts and Wittmann patch tightening. During this time, there were at least two episodes when the abdominal fascia was almost completely approximated. Unfortunately, the patient's hemodynamic status was so tenuous that every attempt to close the abdominal wall resulted in the clinical picture of abdominal compartment syndrome with RVAD suction events and hypotension. Each of these times, the Wittmann patch was loosened, and after optimization of the hemodynamic parameters, another Wittmann patch tightening was attempted without success. We hoped to achieve primary fascial closure, as otherwise, the patient could not be listed for a heart transplant until his abdomen was closed and healed.
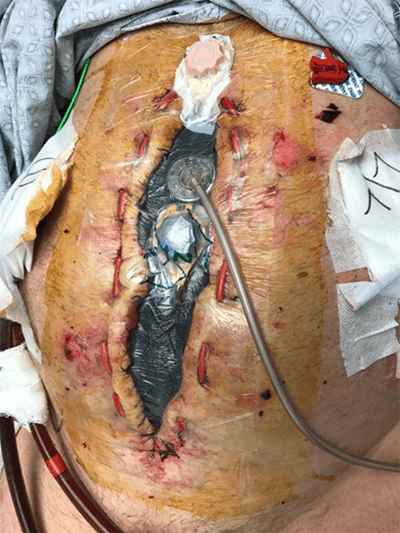
The decision was made to close the abdominal fascia with a biologic mesh and a 20 cm x 40 cm Strattice mesh that was placed in an inlay bridge fashion and sutured to the abdominal wall fascia given the patient's persistently tenuous hemodynamics (Figure 1). The size of the abdominal wall defect (20 cm x30 cm) did not allow us to close the skin primarily even after the creation of bilateral skin flaps. The complicating factor here was the presence of bilateral ECMO cannulas going through the mid-abdomen closely located to the midline laparotomy incision. A negative pressure vacuum dressing was applied on top of the Strattice mesh to cover the skin defect. We assumed that wound vacuum dressing would facilitate the growth of granulation tissue from the skin flaps over the mesh.