Given the severity of abdominal pain and CT scan findings, the patient was admitted to surgery service for observation. Initial treatment included intravenous fluid, pain medication, venous thromboembolic prophylaxis with enoxaparin, prophylactic ceftriaxone and metronidazole, and nil per os. The COVID-19 reverse transcription-polymerase chain reaction (PCR) test produced a positive result soon after surgical evaluation. At this point, our institution's COVID-19 medicine team took over her care while the surgical team monitored her abdominal pain. Additional labs including CRP, ferritin, procalcitonin, LDH, BNP, troponin, D-dimer, fibrinogen and PT/PTT were sent; all were elevated except for troponin and PT/PTT. As part of the treatment algorithm for patients with COVID-19 at our institution, she was treated with hydroxychloroquine for six days and a steroid taper. She was also treated with ceftriaxone and metronidazole for eight days to prevent gastrointestinal bacterial translocation and bacterial pneumonia. The patient continued to have abdominal pain and lacked appetite. She also developed diarrhea. Testing was negative for common sources of infectious diarrhea, including Clostridium difficile, Giardia lamblia, Cryptosporidium, and Norovirus.
On the fourth day of hospitalization, a follow-up abdominal and pelvic CT scan showed interval resolution of previously noted thickened jejunal and ileal loops, decreased pelvic ascites, and resolution of previously seen perihepatic ascites. Regarding her pulmonary status, there was an interval increase in peripheral ground-glass opacities and patchy consolidations, most consistent with COVID-19 related pneumonia. Interestingly, the patient never manifested respiratory signs or other typical symptoms of COVID-19 during her hospitalization. The patient's symptoms improved over the next nine days, her diet was advanced slowly, and she was discharged on hospital day 13 for home isolation.
Discussion
The most common manifestations of COVID-19 include fever, chills, cough, shortness of breath, and fatigue.1–4 Gastrointestinal symptoms such as nausea, vomiting, and diarrhea are less common, and fewer than 10 percent of patients present with abdominal pain.2,5 This case highlights an atypical manifestation of SARS-CoV-19 gastroenteritis that resembled an acute surgical abdomen. SARS-CoV-19 likely enters human host cells through cellular receptor angiotensin-converting enzyme 2 (ACE 2), which is expressed in both intestinal cells and alveolar type 2 cells in the lung. The virus can possibly replicate in the gastrointestinal tract.6,7 Additionally, studies have identified SARS-CoV-2 RNA in stool specimens of infected patients, sometimes even when the nasopharyngeal test returns negative.8
Abdominal pain appears to be the least common manifestation of gastrointestinal involvement, with studies reporting abdominal pain in 2‒6 percent of gastrointestinal presentations in COVID-19 patients.3,7,9 Poggiali et al. recently reported a cohort of ten COVID-19 positive patients presenting with gastrointestinal symptoms of which only one had non-surgical abdominal pain. Saeed et al. further describe nine COVID-19 positive patients presenting with abdominal pain, all of whom were eventually discharged home.10 Sellevoll et al. recently reported a case of acute abdominal pain that was initially suspicious for cholecystitis but was later attributed to COVID-19 upon imaging that was negative for cholecystitis and positive SARS-CoV-19 PCR test.11 Similar to our case, the patient presented by Sellevoll also did not experience respiratory symptoms, but CT scan findings in the lower thorax were consistent with viral pneumonia.
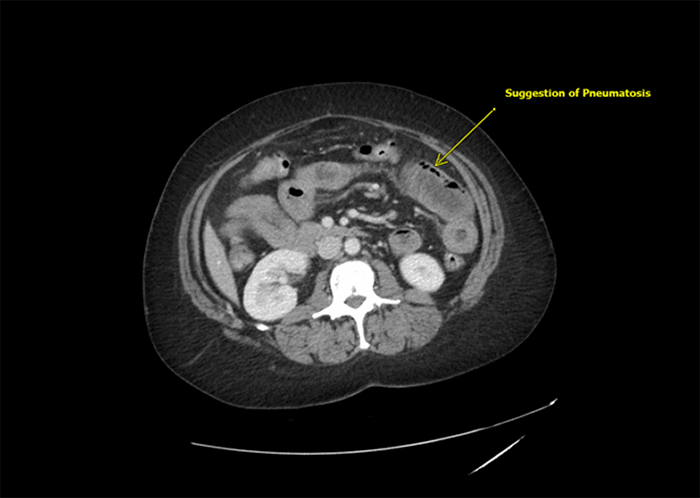
Mesenteric ischemia, which often presents as an acute abdomen, has been reported among patients with COVID-19. Observation of ischemic symptoms and prophylactic anticoagulation therapy have been suggested in these cases.12–15 COVID-19 predisposes patients to a prothrombotic state as evidenced by increases in D-dimer levels and inflammatory markers among those infected.16,17 Therefore, those infected with COVID-19 are at greater risk for venous and arterial thromboembolism.18–20 Although there was no evidence of thromboembolism in the main mesenteric vessels and their major branches on our patient's imaging, the CT scan did raise the possibility of intestinal pneumatosis and ischemia. These intestinal findings had resolved on repeat imaging. Regardless, our patient was treated with prophylactic enoxaparin during the entire hospitalization and as part of the treatment algorithm for patients with COVID-19 infection.
In the ongoing COVID-19 pandemic, surgeons have a continued responsibility in providing acute care for patients, including assessing acute abdominal pain and deciding if surgery is warranted. This case highlights a patient with COVID-19, who presented with only gastrointestinal symptoms suggestive of surgical abdomen that, in the end, did not require surgery. We underscore the importance of including COVID-19 on a differential diagnosis in the setting of an acute abdomen, even in the absence of hallmark symptoms of fever, cough, and shortness of breath.
Conclusion
COVID-19 management is rapidly evolving, but significant knowledge gaps in clinical understanding continue to persist. While most symptomatic patients present with typical signs of fever, cough, fatigue, and muscle ache, a small subset of patients may present with gastrointestinal symptoms only, including acute abdominal pain. This case demonstrates the importance of considering the atypical COVID-19 gastroenteritis in the differential diagnosis for abdominal pain. Awareness of atypical presentations is vital for triage, early treatment, prevention of spread, and streamlined personnel and resource utilization.
Lessons Learned
Gastrointestinal symptoms and abdominal pain may be the sole presentation in a small subset of COVID-19 patients lacking typical symptoms of fever, cough, fatigue, and shortness of breath. Surgeons must be vigilant in evaluating patients with acute abdominal pain in a COVID-19 era.
Authors
Chan SMa; Ying LDb; Morton JMb; Ghiassi Sb
Author Affiliations
- Yale School of Medicine, New Haven, CT, 06510
- Department of Surgery, Yale School of Medicine, New Haven, CT, 06510
Corresponding Author
Saber Ghiassi, MD, MPH, FACS
Yale Bariatric & Minimally Invasive Surgery
2000 Post Road, Ste. 101
Fairfield, CT, 06824
Phone: (203) 418-9520
E-mail: saber.ghiassi@yale.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no financial relationships or in-kind support to disclose.
Received: July 14, 2020
Revision Received: November 1, 2020
Accepted for Publication: November 24, 2020
References
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. doi:10.1056/NEJMoa2002032
- Zhang B, Zhou X, Qiu Y, et al. Clinical characteristics of 82 cases of death from COVID-19. PLoS One. 2020;15(7):e0235458. Published 2020 Jul 9. doi:10.1371/journal.pone.0235458
- Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730-1741. doi:10.1111/all.14238
- Symptoms of COVID-19. Centers for Disease Control and Prevention. Accessed June 16, 2020.
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China [published correction appears in JAMA. 2021 Mar 16;325(11):1113]. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585
- Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-Angiotensin-Aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020;382(17):1653-1659. doi:10.1056/NEJMsr2005760
- Wong SH, Lui RN, Sung JJ. COVID-19 and the digestive system. J Gastroenterol Hepatol. 2020;35(5):744-748. doi:10.1111/jgh.15047
- Yang L, Tu L. Implications of gastrointestinal manifestations of COVID-19. Lancet Gastroenterol Hepatol. 2020;5(7):629-630. doi:10.1016/S2468-1253(20)30132-1
- Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. doi:10.14309/ajg.0000000000000620
- Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T. COVID-19 may present with acute abdominal pain. Br J Surg. 2020;107(7):e186-e187. doi:10.1002/bjs.11674
- Sellevoll HB, Saeed U, Young VS, Sandbæk G, Gundersen K, Mala T. Acute abdomen as an early symptom of COVID-19. Covid-19 med akutte magesmerter som debutsymptom. Tidsskr Nor Laegeforen. 2020;140(7):10.4045/tidsskr.20.0262. Published 2020 Mar 31. doi:10.4045/tidsskr.20.0262
- Vartanoglu Aktokmakyan T, Tokocin M, Meric S, Celebi F. Is mesenteric ischemia in COVID-19 patients a surprise?. Surg Innov. 2021;28(2):236-238. doi:10.1177/1553350620962892
- Rodriguez-Nakamura RM, Gonzalez-Calatayud M, Martinez Martinez AR. Acute mesenteric thrombosis in two patients with COVID-19. Two cases report and literature review. Int J Surg Case Rep. 2020;76:409-414. doi:10.1016/j.ijscr.2020.10.040
- Singh B, Mechineni A, Kaur P, et al. Acute intestinal ischemia in a patient with COVID-19 infection. Korean J Gastroenterol. 2020;76(3):164-166. doi:10.4166/kjg.2020.76.3.164
- Parry AH, Wani AH, Yaseen M. Acute mesenteric ischemia in severe coronavirus-19 (COVID-19): possible mechanisms and diagnostic pathway. Acad Radiol. 2020;27(8):1190. doi:10.1016/j.acra.2020.05.016
- Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed [published correction appears in Nat Rev Immunol. 2020 Jun 4;:]. Nat Rev Immunol. 2020;20(7):389-391. doi:10.1038/s41577-020-0343-0
- Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033-2040. doi:10.1182/blood.2020006000
- Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. doi:10.1016/j.thromres.2020.04.013
- Moll M, Zon RL, Sylvester KW, et al. VTE in ICU patients with COVID-19. Chest. 2020;158(5):2130-2135. doi:10.1016/j.chest.2020.07.031
- Cheruiyot I, Kipkorir V, Ngure B, Misiani M, Munguti J, Ogeng'o J. Arterial thrombosis in coronavirus disease 2019 patients: a rapid systematic review. Ann Vasc Surg. 2021;70:273-281. doi:10.1016/j.avsg.2020.08.087