Discussion
Despite the recent advances in genetics, chemotherapy, radiation therapy, and surgery, there were approximately 42,260 deaths from breast cancer in 2019.1,2 The majority of patients will die from metastases. The two most common types of breast cancer, invasive ductal carcinoma (70‒80 percent) and lobular (10‒15 percent), have different routes of metastases.3,4 Ductal carcinoma more typically metastasizes to the brain, lung, and liver, whereas lobular carcinoma more commonly metastasizes to the bones and less commonly to the gastrointestinal (GI) tract.5 Malignant melanoma is the most common primary to metastasize to the GI tract.6 We are reporting on a recent case of breast metastasis to the anal canal in a young female from an invasive ductal carcinoma masquerading as a thrombosed external hemorrhoid
Metastatic breast cancer to the gastrointestinal tract is rare. In a series of 12,001 patients, McLemore found only 73 patients with metastatic disease to the GI tract, including 23 in a group with GI metastases only and 18 with GI metastases and carcinomatosis. The majority of metastases were infiltrating lobular cancer of the breast. The mean interval between the primary diagnoses and metastatic presentation was seven years. The most common site was the colon and rectum (45 percent), followed by the stomach (28 percent). There were no metastases to the anal canal. The median overall survival after diagnosis was 28 months.7 In contrast to previous studies, Mourra found that in a study of 10,365 patients with colorectal cancer, 35 were found to be metastatic, interestingly the most common being breast cancer followed by melanoma, lung, and sarcoma.8
Anal metastases are most rare. The first reported case was reported by Dawson et al. in 1985 of a 70-year-old with invasive lobular carcinoma breast metastases to the anal canal.9 Since then, there have been seven case reports of anal metastases from metastatic breast carcinoma worldwide; four with lobular cancer and three with invasive ductal carcinoma.9‒16 Only one was treated by extirpation.10 Two were treated with colostomy because of possible obstruction.11,13 The patient who underwent resection was disease-free two years later. None presented as a possible thrombosed external hemorrhoid or an anal margin lesion. Their survival time from diagnosis of the anal metastases ranged from a few months to three years.10‒15 The survival time for patients with IDC is unknown, but this patient survived three months, which supports the grave prognosis with this finding.15
Table. Reported Cases of Anal Metastasis from Breast Carcinoma
Case |
Age (years)
|
Histology
|
Interval
|
Clinical presentation
|
Therapy
|
Survival
|
|
Dawson et al.9
|
70
|
ILC
|
34 months
|
Altering bowel habit, constipation, anal discharge
|
Laparotomy and RT
|
N/A
|
|
Haberstich et al.10
|
78
|
IDC
|
At diagnosis
|
Painful anal tumefaction and blood loss with stools
|
Abdominoperineal resection and RT
|
Disease-free at 22 months follow-up
|
|
Nair et al.11
|
57
|
IDC
|
7 years
|
Alternating bowel habit, crampy lower abdominal pain, increased frequency of bowel movements
|
Colostomy and RT
|
N/A
|
|
Puglisi et al.12
|
92
|
ILC
|
4 years
|
Tenesmus and painful anal polypoid lesion
|
RT and hormonal therapy
|
3 years
|
|
Bochicchio et al.13
|
72
|
ILC
|
4 years
|
Constipation, tenesmus, fecal incontinence
|
Hartmann rectal amputation and RT
|
Few months after RT
|
|
Rengifo et al.14
|
78
|
IDC
|
27 months before diagnosis of BC
|
Rectal bleeding, weight loss, constipation
|
RT and hormonal therapy
|
N/A
|
|
Ruymbeke et al.15
|
65
|
ILC
|
4 years
|
stool, intermittent fecal incontinence and tenesmus
|
Hormonal therapy and chemotherapy
|
Alive after 15 months
|
|
Hasan et al.
|
35
|
IDC
|
5 years
|
External hemorrhoid, rectal pain and pressure
|
Chemotherapy, conservative
|
3 months
|
Adapted from Ruymbeke et al. with permission from authors
Traditional universal medical school training has taught that every physical examination always includes a rectal exam; however, this may have fallen by the wayside. This lesion was noted but undiagnosed by physicians for at least one month. Had she been diagnosed with an anal metastasis earlier, would that have made a difference in her overall course? In this case, no. Had the surgeon proceeded in treating the lesion as a thrombosed external hemorrhoid, would the patient have been harmed? In this case, yes. Total excision of the lesion without recognizing this as a metastasis would have led to a morbid, painful, non-healing wound at a time when the quality of life is paramount. Misdiagnosis, therefore, can be avoided with appropriate knowledge of patient history and a high index of suspicion.
In cancer patients who are opioid-dependent, hemorrhoids brought on by relentless constipation are far too common. Diagnosis, therefore, requires a high level of suspicion, knowledge of the patient, and a thorough physical exam. When the diagnosis is made, options should be discussed with the patient, understanding that there are limited treatment options versus palliative care. If isolated and limited in size, resection may not lead to morbidity and could be considered. In this case, resection would have created a very morbid wound and was avoided because it was recognized as atypical.
Conclusion
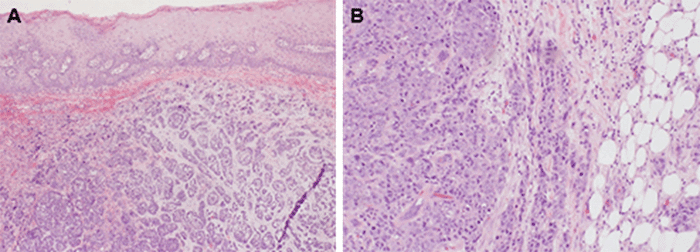
Patients with advanced breast cancer may also present with metastases to the anus. Although lobular carcinoma is more likely to metastasize to the GI tract, ductal carcinoma, as evidenced by this case, also has this metastatic potential. Acute presentation with pain does not rule out the diagnosis. Thorough knowledge of patient history remains important in treating patients with all conditions, including anal pathology. Surgeons should have a low threshold for excision/biopsy and pathologic confirmation in patients with interval development of anal pathology and history of malignancy, including breast. This represents the first case report of ductal carcinoma with metastasis to the anal margin initially misdiagnosed as a thrombosed external hemorrhoid.
Lessons Learned
Appearances may be deceiving when assessing anorectal pathology. A thorough understanding of a patient history remains important. Ductal carcinoma of the breast can metastasize to the anus and present similar to a thrombosed external hemorrhoid. In general, gastrointestinal metastases of breast cancer portend a poor prognosis.
Authors
Hasan SY; Fischer JL; Tsoraides SS; Bonello JP; Mammolito DM
Author Affiliations
Department of Surgery, University of Illinois College of Medicine, Peoria, IL 61603
Corresponding Author
Syeda A. Hasan, MD
Department of Surgery
University of Illinois College of Medicine
624 NE Glen Oak Avenue
Peoria, IL 61603
Phone: (630) 242-0091
E-mail: hasan7@uic.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no financial relationships or in-kind support to disclose.
Received: July 6, 2019
Revision Received: May 17, 2020
Accepted for Publication: October 29, 2020
References
- DeSantis CE, Ma J, Goding Sauer A, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017;67(6):439-448. doi:10.3322/caac.21412
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7-34. doi:10.3322/caac.21551
- Li CI, Anderson BO, Daling JR, Moe RE. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA. 2003;289(11):1421-1424. doi:10.1001/jama.289.11.1421
- Li CI, Uribe DJ, Daling JR. Clinical characteristics of different histologic types of breast cancer. Br J Cancer. 2005;93(9):1046-1052. doi:10.1038/sj.bjc.6602787
- Mathew A, Rajagopal PS, Villgran V, et al. Distinct pattern of metastases in patients with invasive lobular carcinoma of the breast. Geburtshilfe Frauenheilkd. 2017;77(6):660-666. doi:10.1055/s-0043-109374
- Jain S, Fisher C, Smith P, Millis RR, Rubens RD. Patterns of metastatic breast cancer in relation to histological type. Eur J Cancer. 1993;29A(15):2155-2157. doi:10.1016/0959-8049(93)90053-i
- McLemore EC, Pockaj BA, Reynolds C, et al. Breast cancer: presentation and intervention in women with gastrointestinal metastasis and carcinomatosis. Ann Surg Oncol. 2005;12(11):886-894. doi:10.1245/ASO.2005.03.030
- Mourra N, Jouret-Mourin A, Lazure T, et al. Metastatic tumors to the colon and rectum: a multi-institutional study. Arch Pathol Lab Med. 2012;136(11):1397-1401. doi:10.5858/arpa.2011-0432-OA
- Dawson PM, Hershman MJ, Wood CB. Metastatic carcinoma of the breast in the anal canal. Postgrad Med J. 1985;61(722):1081. doi:10.1136/pgmj.61.722.1081
- Haberstich R, Tuech JJ, Wilt M, Rodier JF. Anal localization as first manifestation of metastatic ductal breast carcinoma. Tech Coloproctol. 2005;9(3):237-238. doi:10.1007/s10151-005-0235-0
- Nair M, Fafemi O. Anorectal metastasis from breast carcinoma: a case report with literature review. Internet J Oncol. 2007;5(2).
- Puglisi M, Varaldo E, Assalino M, Ansaldo G, Torre G, Borgonovo G. Anal metastasis from recurrent breast lobular carcinoma: a case report. World J Gastroenterol. 2009;15(11):1388-1390. doi:10.3748/wjg.15.1388
- Bochicchio A, Tartarone A, Ignomirelli O, et al. Anal metastasis from breast cancer: a case report and review of the literature. Future Oncol. 2012;8(3):333-336. doi:10.2217/fon.12.9
- Rengifo C, Titi S, Walls J. Anal metastasis as the sentinel and isolated presentation of invasive ductal breast carcinoma. Ann R Coll Surg Engl. 2016;98(5):e68-e70. doi:10.1308/rcsann.2016.0108
- Ruymbeke H, Harlet L, Stragier B, Steenkiste E, Ryckx M, Marolleau F. Anorectal metastasis from breast carcinoma: a case report and review of the literature. BMC Res Notes. 2018;11(1):268. Published 2018 May 2. doi:10.1186/s13104-018-3356-z