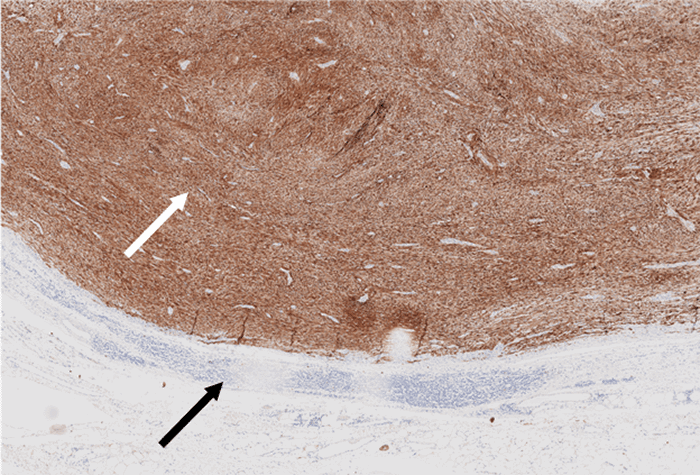
Tumor (white arrow) is diffusely positive for S100, supporting assumption of benign schwannoma; by contrast, malignant peripheral nerve sheath tumors only show focal S100 positivity—adjacent capsule and lymphatic cuff (black arrow) show no immunoreactivity
Discussion
Adrenal incidentalomas are adrenal tumors discovered on an imaging study obtained for indications exclusive to adrenal conditions.1,2 A radiological pre-requisite for an adrenal tumor to be considered an incidentaloma is that the tumor must be greater than 1 cm in maximum diameter.3
The majority of resected incidentalomas are non-functioning cortical adenomas. Differential diagnoses can include benign diagnoses, such as nodular hyperplasia, myelolipoma, ganglioneuroma, hamartoma, hemangioma, leiomyoma, neurofibroma, and teratoma. However, potentially malignant neoplasms, such as pheochromocytoma and primary ACC, are high on differential diagnoses, especially in larger tumors with atypical imaging characteristics.1,4 In studies correlating radiological and pathological adrenal tumor characteristics, the prevalence of adrenal incidentalomas has been noted to be approximately 5 percent, with fewer than 10 percent demonstrating endocrine functionality and fewer than 5 percent malignant. Adrenocortical adenoma is the most common tumor type, with prevalence estimates ranging from 1.4 to 8.9 percent based on autopsy series.5,6 In another recent study, the prevalence of adrenal incidentalomas was noted to be four percent in middle-age and up to ten percent in the elderly. In 80 percent of the cases, the final diagnosis was a non-functional benign adenoma. Despite differences in the reported prevalence, the most common functional, although often asymptomatic, incidentaloma is pheochromocytoma, comprising 11–23 percent of incidental adrenal tumors.7
Schwannomas are benign nerve sheath tumors thought to arise from peripheral, motor, sympathetic, or cranial nerves of the head and neck region and upper and lower extremities. They are usually solitary tumors in the gastrointestinal tract derived from the Auerbach and the Meissner myenteric plexus. They are located primarily in the stomach as submucosal lesions, often challenging to differentiate from gastrointestinal stromal tumors.8,9 Schwannomas presenting in the adrenal gland, however, are quite uncommon. The innervation of the adrenal medulla is comprised of the phrenic nerve, the vagus nerve, and the sympathetic trunk, from which adrenal schwannomas are thought to arise.10 Malignant peripheral nerve sheath tumors (MPNSTs) are also very rare, comprising only 2 percent of all soft tissue sarcomas. MPNSTs are usually associated with neurofibromatosis type I syndrome and are almost always diagnosed on final microscopic histopathology and immunohistochemistry.11,12
To date, fewer than 50 cases of adrenal schwannomas have been reported in the literature. Almost all are non-functional tumors, except a single case report of an adrenal retroperitoneal schwannoma with catecholamine overproduction and oversecretion.13 Recognizing an adrenal schwannoma based on imaging features is very challenging, and the potential for malignancy is difficult to exclude. Thus, surgical resection is almost always the recommended approach, either open or laparoscopic, depending on size and on preoperative concerns for malignancy and surgeon preference.1,14–16
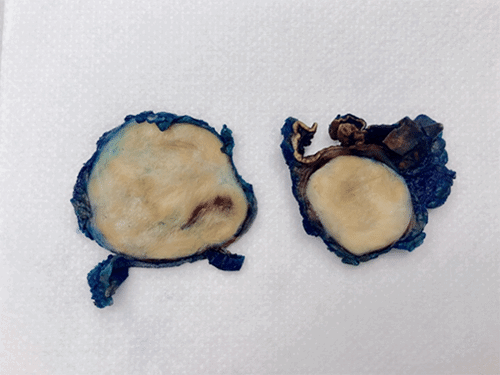
Gross and microscopic pathology of adrenal schwannoma typically reveal a firm, well-circumscribed rounded mass, tan-yellow to grayish-white in appearance, which can appear heterogeneous when larger in size (Figure 4). Adrenal schwannomas may or may not have a fibrous capsule but overall appear grossly similar to schwannomas originating from other sites. Immunohistochemistry stains are consistent with benign peripheral nerve sheath tumors, almost always with S-100 diffuse positivity, which differentiates these tumors from pheochromocytomas. Schwannomas are also characteristically negative for CD117, desmin, CD-34, HMB-45, synaptophysin, chromogranin, cytokeratin, and smooth muscle actin.10,14
Figure 4. Gross Photograph of Specimen, Showing Normal Grayish-White Appearance of Benign Schwannoma. Published with Permission