Discussion
Obturator hernias are an infrequently described, with incidence estimates below 1 percent of all hernias.1 They can be a dangerous cause of bowel obstruction, often undiagnosed until intestinal ischemia and gangrene have occurred.1‒3 The classic teaching is that these hernias are found in thin, frequently multiparous, and older women, manifesting as intestinal obstruction.4 They start as an invagination of the preperitoneal fat that is the precursor to a true hernia that may contain bowel, leading to the classic symptoms of discomfort and obstruction.4 Surgery is the gold standard in the definitive management of obturator hernia,5 although the best approach has not been settled. If a diagnosis is made early, significant mortality and morbidity can be avoided and allow for minimally invasive methods to resolve the hernia.
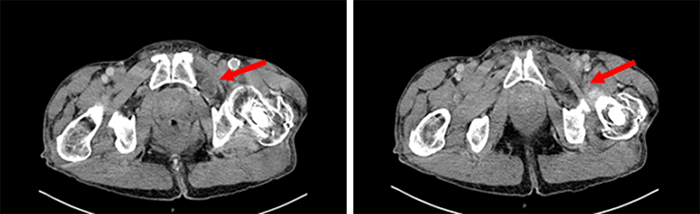
Due to their rarity, obturator hernias can present a diagnostic challenge unless a high index of suspicion is maintained. Our patient presented with nonspecific symptoms that were originally attributed to hip disease, which can be a classic presenting finding per review of the literature.6,7 It is possible that our patient noted discomfort at the early 'fat plug'4 stages of obturator hernia, avoiding the invagination of the intestine that frequently leads to strangulation and incarceration.5 Early diagnosis is a rare phenomenon, contributing to the relatively high mortality rate seen with this type of abdominal wall hernias.8
The decision was made to allow the patient to present for elective hernia repair as his obstructive symptoms resolved while in observation. The bowel was viable at diagnostic laparoscopy, so minimally invasive repair with mesh placement was reasonable. We pursued an extraperitoneal repair for this case due to our familiarity with the approach and the ability to repair both inguinal and obturator spaces without further entry into the peritoneum.
Conclusion
A high index of suspicion must be maintained to diagnose obturator hernias, but the increase in the use of CT in emergency departments has aided their discovery. If the bowel is healthy and viable at the time of operation, it is appropriate to pursue laparoscopic repair for these patients due to the decreased recovery time and ability to assess other possible hernia sites bilaterally.
Lessons Learned
Although obturator hernias are a rare cause of intestinal obstruction, keeping a high index of suspicion on evaluation can allow for early diagnosis and minimally invasive repair.
References
- Lo CY, Lorentz TG, Lau PW. Obturator hernia presenting as small bowel obstruction. Am J Surg. 1994;167(4):396-398. doi:10.1016/0002-9610(94)90123-6
- Yokoyama Y, Yamaguchi A, Isogai M, Hori A, Kaneoka Y. Thirty-six cases of obturator hernia: does computed tomography contribute to postoperative outcome?. World J Surg. 1999;23(2):214-217. doi:10.1007/pl00013176
- Karasaki T, Nomura Y, Tanaka N. Long-term outcomes after obturator hernia repair: retrospective analysis of 80 operations at a single institution. Hernia. 2014;18(3):393-397. doi:10.1007/s10029-013-1159-7
- Susmallian S, Ponomarenko O, Barnea R, Paran H. Obturator hernia as a frequent finding during laparoscopic pelvic exploration: A retrospective observational study. Medicine (Baltimore). 2016;95(27):e4102. doi:10.1097/MD.0000000000004102
- Leitch MK, Yunaev M. Difficult diagnosis: strangulated obturator hernia in an 88-year-old woman. BMJ Case Rep. 2016;2016:bcr2016215428. Published 2016 Jun 29. doi:10.1136/bcr-2016-215428
- Belli AK, Memiş G, Dere Ö, Koşan U, Nazlı O. Obturator hernia should be considered in the differential diagnosis of hip and knee pain. Ulus Travma Acil Cerrahi Derg. 2016;22(6):575-577. doi:10.5505/tjtes.2016.91582
- Tateno Y, Adachi K. Sudden knee pain in an underweight, older woman: obturator hernia. Lancet. 2014;384(9938):206. doi:10.1016/S0140-6736(14)60883-7
- Rito CC, Travassos J, Patrã cio J, Duarte AL. Obturator hernia: a rare cause of bowel obstruction. BMJ Case Reports. 2017. doi:10.1136/bcr-2017-219369.
Authors
Nielsen DJ; Holkup LM; Seiler J; Kroetsch CJ
Author Affiliation
Department of Surgery, VA Medical Center Fargo, Fargo, ND 58102
Corresponding Author
Corey J. Kroetsch, MD
Department of Surgery
VA Medical Center Fargo
2101 Elm Street N
Fargo, ND 58102
Phone: (701) 232-3241
Email: corey.kroetsch@und.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: August 20, 2020
Revision received: October 1, 2020
Accepted: November 1, 2020