Discussion
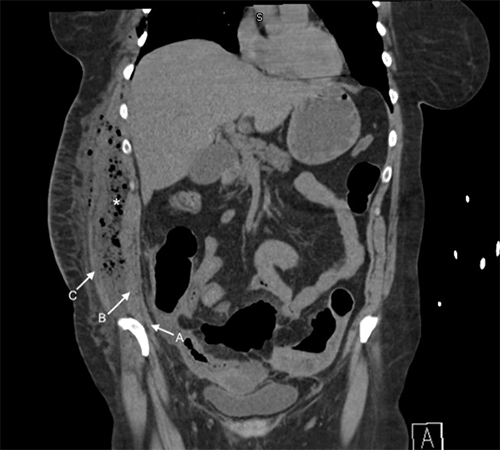
Adriaan van der Spieghel, a Belgian anatomist, first described the semilunar line in 1645. Still, it was Josef Klinkosch who defined the Spigelian hernia as a defect through the linea semilunaris in 1764.1,4 SH remains a rare presentation of abdominal wall hernias. Around 90% of SHs occur in the Spigelian belt, a 6 cm region along the Spigelian aponeurosis starting below the level of the umbilicus and spanning to the interspinal plane.1‒3 Above the semicircular line of Douglas, the hernia may extend through one, two, or all three muscular layers of the transversus abdominus, internal oblique, and external oblique.1 In this patient's case, the hernia extended through the first two layers, permitting the infection to enter and spread in the potential space between the internal and external oblique.
Although conflicting data exist, several reports show a higher incidence of SH in females.2,3 Most diagnoses occur in patients in their fifth or sixth decade of life. Risk factors associated with the development of SH include obesity, multiple pregnancies, chronic pulmonary obstructive disease, and smoking.2,3,5 Common presentation of SH includes vague abdominal pain or bulging mass lateral and inferior to the umbilicus, more often on the right side.2,3 Usually, the hernia does not extend through the external oblique, adding difficulty to the clinical diagnosis of smaller, asymptomatic SH.7 Sonography and CT have high sensitivity and positive predictive value in identifying occult SHs.7 Contents of hernia usually include omentum and small bowel. A review of literature has revealed several unusual clinical presentations of SH, including contained appendicitis, endometriosis, gallbladder volvulus, and incarcerated Meckel's diverticulum contained within the hernia sac.5,6,8 There has been no prior report of necrotizing infection traversing the abdominal wall through a Spigelian hernia. In the setting of undiagnosed Spigelian hernia, intraabdominal infection such as perforated diverticulitis could provide a path for infection to spread to external abdominal wall musculature, as seen in this patient.
Conclusion
This case report describes an unusual etiology of necrotizing abdominal and chest wall infection. There should be clinical suspicion for a Spigelian hernia when concurrent infection occurs in the abdominal cavity and external abdominal musculature, especially along the right side.
Lessons Learned
Spigelian hernias, although uncommon, may present in numerous ways, including incarceration and bowel strangulation. Understanding the anatomical etiology of these hernias is critical in understanding the spread of intra-abdominal infection in this rare progression from diverticulitis to a right flank necrotizing soft tissue infection.
References
- Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72(1):42-48.
- Polistina FA, Garbo G, Trevisan P, Frego M. Twelve years of experience treating Spigelian hernia. Surgery. 2015;157(3):547-550. doi:10.1016/j.surg.2014.09.027
- Cinar H, Polat AK, Caglayan K, Ozbalci GS, Topgül HK, Polat C. Spigelian hernia: our experience and review of the literature. Ann Ital Chir. 2013;84(6):649-653.
- Ghosh SK, Sharma S, Biswas S, Chakraborty S. Adriaan van den Spiegel (1578-1625): anatomist, physician, and botanist. Clin Anat. 2014;27(7):952-957. doi:10.1002/ca.22414
- Thomas MP, Avula SK, England R, Stevenson L. Appendicitis in a Spigelian hernia: an unusual cause for a tender right iliac fossa mass. Ann R Coll Surg Engl. 2013;95(4):e66-e68. doi:10.1308/003588413X13511609957731
- Donati M, Brancato G, Scilletta R, Deiana E, Basile G. A surgical "chimera": the gallbladder volvulus in the Spigelian hernia sac Am Surg. 2017;83(1):e11-e12.
- Light D, Chattopadhyay D, Bawa S. Radiological and clinical examination in the diagnosis of Spigelian hernias. Ann R Coll Surg Engl. 2013;95(2):98-100. doi:10.1308/003588413X13511609957092
- Moris D, Michalinos A, Vernadakis S. Endometriosis in a Spigelian hernia sac: an unexpected finding. Int Surg. 2015;100(1):109-111. doi:10.9738/INTSURG-D-13-00245.1
Authors
Wang YHWa; Albright JBb
Author Affiliations
- Icahn School of Medicine at Mount Sinai, New York, NY 10029
- Department of Surgery, State University of New York Upstate Medical University, Syracuse, NY 13210
Corresponding Author
Jeffrey B. Albright, MD, MBA, FACS, FASCRS
Department of Surgery
State University of New York Upstate Medical University
750 E. Adams Street, Ste. 8140
Syracuse, NY 13210
Phone: (315) 464-6292
Email: albrighj@upstate.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: August 9, 2019
Revision received: December 13, 2020
Accepted: December 14, 2020