Discussion
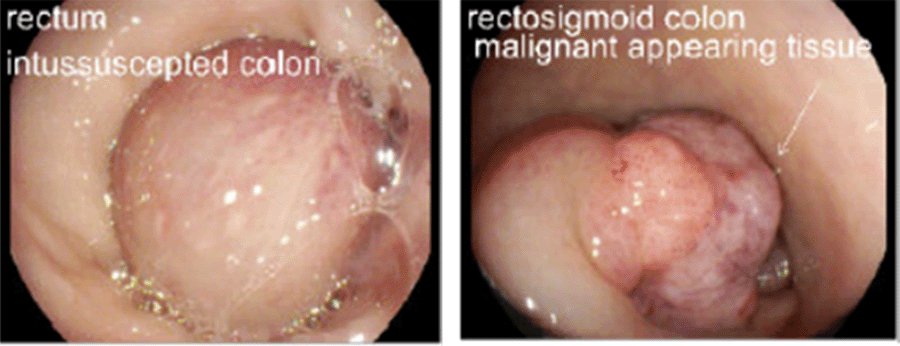
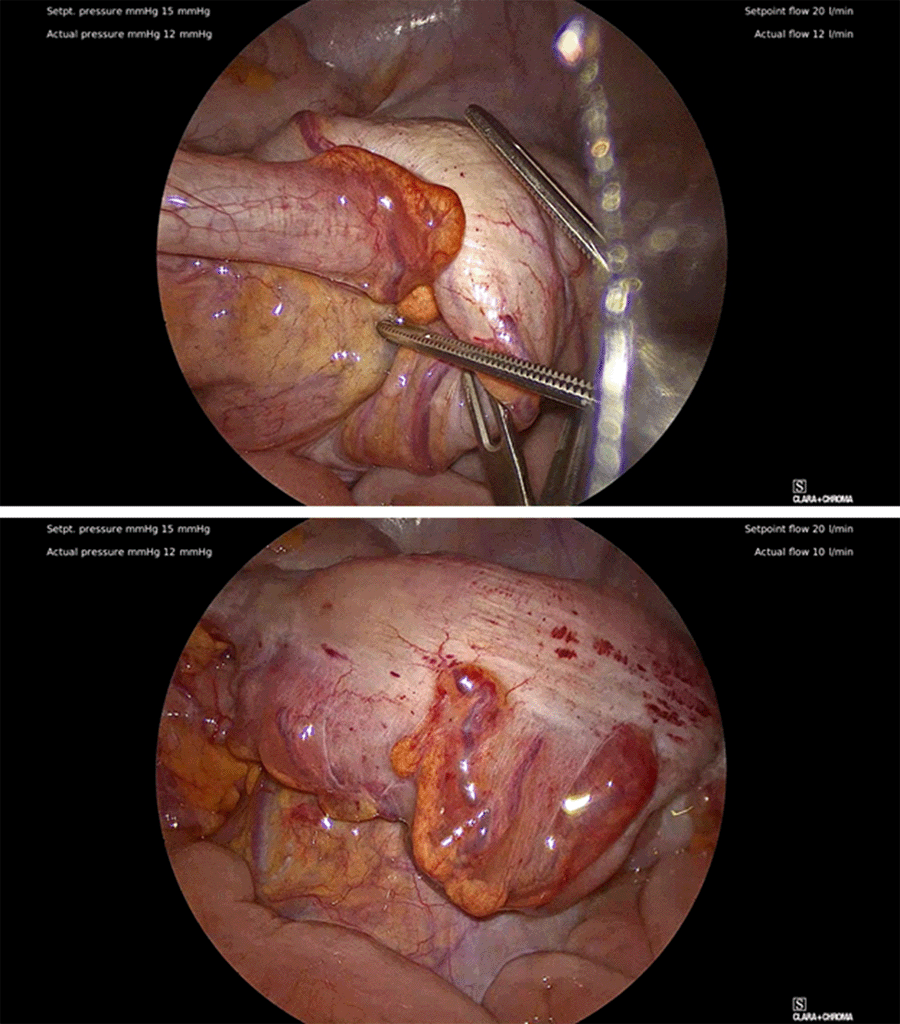
RSI, a rare form of adult intussusception, poses a diagnostic and management dilemma for the clinician. The urgent need for intervention and providing definitive treatment makes surgical planning difficult as decisions on operative approach and reduction are subject to limited data and surgeon experience.3 Critical to this patient's management was urgent surgical intervention after confirmation of diagnosis. The case demonstrates a safe and feasible approach to an oncologic RSI in an urgent setting, incorporating reduction of the intussusception before oncologic resection and protective diverting ileostomy.
The utility of reducing the intussusception prior to resection remains controversial, as the risk of iatrogenic bowel perforation during manipulation can propagate profound sepsis from bowel spillage or carcinomatosis.4,5 Based on these risks, some authors have advocated against a reduction of the intussuscepted bowel.6‒8 Conversely, others maintain a safe reduction of the intussusception, allowing for margin delineation and characterization of the lead point while avoiding excessive bowel resection. Matsuda et al. described a case of a sigmoid adenocarcinoma RSI that had intussuscepted through the rectum into the anal canal, managed by reduction of the RSI before resection allowing avoidance of an abdominoperineal resection.9 Additionally, Greenley et al. described a case of RSI managed by laparoscopic sigmoidectomy after reduction, maintaining that proceeding directly to resection may have necessitated the need for colostomy while acknowledging that surgeons should use this technique with proficiency in minimally invasive techniques.10 Our case supports Matsuda's and Greenley's approach and facilitated resection with primary anastomosis and optimized healing.
Second, there is a growing body of evidence to support the utility of laparoscopy in intussusception.11‒13 Krane et al., in a meta-analysis on rectal cancer, found laparoscopic LAR reduced blood loss, facilitated the earlier return of bowel function, decreased length of stay, and resulted in non-inferior oncologic outcomes compared to an open approach.14 Additional reports from Park et al. and Chuang et al. described cases of RSI secondary to malignancy managed with laparoscopic reduction and resection, lending credibility to this technique.11,12 Given the hemodynamic stability in our case and no concern for compromised bowel, we proceeded with a laparoscopic approach that contributed to the patient's recovery and discharge.
Finally, the decision to proceed with temporary diverting ileostomy was multifactorial. Although RSI represents a rare manifestation of colorectal cancer, the decision to proceed with a proximal diversion to protect the anastomosis remains controversial in obstructing cancer and has been reported to be associated with higher rates of complication, infection, and readmission.15 Ultimately, the formation of a protective diverting ileostomy is based on surgeon judgment and clinical scenario. Given the patient's presentation, the conditions that led to diversion included the urgency of the operation, obstructive symptoms, presence of proximal stool burden, and concern for malnutrition, given the patient's recent weight loss. Furthermore, the postoperative recovery and satisfactory outcomes in this case of RSI demonstrated that proximal diversion is a reasonable surgical option when deemed appropriate by the surgeon.
Conclusion
We present the case of an RSI managed with laparoscopic reduction and resection. While not without risks, reduction facilitated formal oncologic resection while optimizing the preservation of the anal sphincter complex.
Lessons Learned
Management of malignant RSI poses several issues for the surgeon when attempting oncologic resection. Although the case demonstrated a safe and effective surgical approach to this rare manifestation of colorectal cancer, further studies are required to formulate definitive guidelines on appropriate surgical approach and diversion.
References
- Alexander R, Traverso P, Bolorunduro OB, et al. Profiling adult intussusception patients: comparing colonic versus enteric intussusception. Am J Surg. 2011;202(4):487-491. doi:10.1016/j.amjsurg.2011.02.006
- Golemi I, Salazar Adum JP, Tafur A, Caprini J. Venous thromboembolism prophylaxis using the Caprini score. Dis Mon. 2019;65(8):249-298. doi:10.1016/j.disamonth.2018.12.005
- Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15(4):407-411. doi:10.3748/wjg.15.407
- Bail JP, Holderbach LJ, Robaszkiewicz M, Dartoy C, Noundou PM, Charles JF. Invagination colique primitive de l'adulte, procidente à l'anus. Deux observations [Primary colonic intussusception protruding from the anus in adults. Two cases]. Ann Radiol (Paris). 1992;35(4):249-254.
- Reis LD, Matos JR, Soares PN, et al. Coloanal intussusception in adults due to lipoma. J. Coloproctology. 2018;38(03):250-253. doi:10.1016/j.jcol.2018.05.002.
- Hong KD, Kim J, Ji W, Wexner SD. Adult intussusception: A systematic review and meta-analysis. Tech. Coloproctol. 2019;23(4):315-324. doi:10.1007/s10151-019-01980-5.
- Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193(2):230-236. doi:10.1097/00000658-198102000-00019
- Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical relevance. Radiol Clin North Am. 2003;41(6):1137-1151. doi:10.1016/s0033-8389(03)00116-7
- Matsuda K, Suda K, Tamura K, et al. Surgical management of adult sigmoid colon intussusception caused by a malignant tumor: report of a case. Surg Today. 2003;33(10):768-771. doi:10.1007/s00595-003-2579-2
- Greenley CT, Ahmed B, Friedman L, Deitte L, Awad ZT. Laparoscopic management of sigmoidorectal intussusception. JSLS. 2010;14(1):137-139. doi:10.4293/108680810X12674612015184
- Park KJ, Choi HJ, Kim SH, et al. Sigmoidorectal intussusception of adenoma of sigmoid colon treated by laparoscopic anterior resection after sponge-on-the-stick-assisted manual reduction. World J Gastroenterol. 2006;12(1):146-149. doi:10.3748/wjg.v12.i1.146
- Chuang Ch, Hsieh C, Lin Ch, Yu J. Laparoscopic management of sigmoid colon intussusception caused by a malignant tumor: case report. Rev Esp Enferm Dig. 2007;99(10):615-616. doi:10.4321/s1130-01082007001000013
- Lee SY, Park WC, Lee JK, Kang DB, Kim Y, Yun KJ. Laparoscopic treatment of adult sigmoidorectal intussusception caused by a mucinous adenocarcinoma of the sigmoid colon: a case report. J Korean Soc Coloproctol. 2011;27(1):44-49. doi:10.3393/jksc.2011.27.1.44
- Krane MK, Fichera A. Laparoscopic rectal cancer surgery: where do we stand?. World J Gastroenterol. 2012;18(46):6747-6755. doi:10.3748/wjg.v18.i46.6747
- Shwaartz C, Fields AC, Prigoff JG, Aalberg JJ, Divino CM. Should patients With obstructing colorectal cancer have proximal diversion?. Am J Surg. 2017;213(4):742-747. doi:10.1016/j.amjsurg.2016.08.005
Authors
Nigam Aa; Holleran Ta; Ko Kb; Houlihan Ba; Bayasi Ma
Author Affiliations
- Department of Surgery, Medstar Georgetown University Hospital, Washington, DC 20007
- Department of Pathology, Medstar Georgetown University Hospital, Washington, DC 20007
Corresponding Author
Mohammed Bayasi, MD
Department of Surgery
Medstar Georgetown University Hospital
3800 Reservoir Rd NW, Fourth Floor
Washington, DC 20007
Phone: (202) 295-0560
Email: mohammed.bayasi@medstar.net
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: August 14, 2020
Revision received: October 26, 2020
Accepted: November 16, 2020