Discussion
Surgeons previously debated the comparative effectiveness of endovascular and open approaches in managing visceral artery aneurysms.2,3,11 With one in four VAAs estimated to present as a life-threatening rupture, a consensus was urgently needed.3 At the time of surgery, a committee of experts within the Society of Vascular Surgery had not yet established consensus guidelines on VAA management. However, the Society's recent recommendations were updated in July 2020. With continued expansion and risk of rupture, repair is recommended for all true SMAA and pseudoaneurysms at the time of diagnosis.11 Endovascular therapy has now evolved into the "first approach" for SMAA repair, given the minimally invasive nature, shorter recovery time, and lower risk of morbidity and death compared to open surgery.2,9‒11 The ability to treat endovascularly revolves around embolization, coiling and/or covered stent placement. However, EVT is limited by the technician's knowledge, anatomic location, collateralization, and patient factors. Open repair allows ligation, total or partial excision and patching, primary repair, plication, and ex vivo reconstruction. An expansion of hybrid suites has led to an increase in on-table conversion to open if either EVT is too difficult to be performed or a contraindication exists, as in this case.
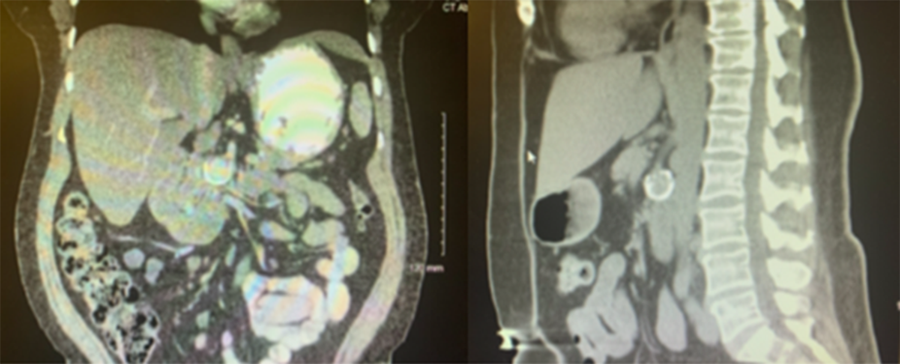
The patient's celiac occlusion limited her EVT options. Coil packing her aneurysm alone could have occluded the outflow tract with subsequent potential for developing catastrophic ischemia along the retrograde path. Alternatively, stenting across the aneurysm was considered, but concern over later occlusion was again deemed unsafe in the setting of celiac occlusion. In a recent study, the one-year primary patency rate of visceral vessel stenting in the setting of mesenteric ischemia was 65%.5 Another study reported a one-year failure rate of approximately 30%.5,6 Finally, a combination of celiac angioplasty with stenting and SMA stenting was ruled out in favor of an open approach over patency and feasibility concerns. Duplex surveillance of three-year primary patency rates after mesenteric revascularization has been reported to be 62% after EVT and 82% after surgical bypass.7,8 Despite these reported patency and failure rates, EVT would have still been preferred if proper collateralization existed due to the decreased morbidity compared to open procedures. The overall mortality from elective repair of SMAA is <15%.
Alternatively, median arcuate ligament syndrome (MALS) should be considered in cases of distal SMAA and, more commonly, pancreaticoduodenal artery and gastroduodenal aneurysms. Ideally, transabdominal duplex ultrasound would have been performed in addition to the CTA assessment, as it is a dynamic study accounting for diaphragm changes during respiration. Our patient had no evidence of crura hypertrophy or diaphragmatic compression on preoperative imaging. Therefore, median arcuate ligament release was not considered at the time of surgery; however, MALS should be ruled out during applicable VAA workup.11 Our patient's request limited our immediate conversion to open therapy as an adjunct to our "EVT first approach." Following bypass of the excised aneurysm, our patient will require annual CTA surveillance as recommended by the Society of Vascular Surgeons.11
Conclusion
Visceral artery aneurysms remain a rare clinical entity. This case underscores the importance of attention to the collateral vascular networks observed during angiography and may provide an additional framework for the continued development of treatment protocols for VAA.
Lessons Learned
Superior mesenteric artery aneurysms should be treated with EVT as the first approach. Prior to EVT therapy, careful attention must be given to vascular collateral networks. Open procedures may be required, as in this case, if embolization, coiling, and/or covered stent therapy is contraindicated.
References
- Barrionuevo P, Malas MB, Nejim B, et al. A systematic review and meta-analysis of the management of visceral artery aneurysms. J Vasc Surg. 2019;70(5):1694-1699. doi:10.1016/j.jvs.2019.02.024
- Obara H, Kentaro M, Inoue M, Kitagawa Y. Correction to: Current management strategies for visceral artery aneurysms: an overview. Surg Today. 2020;50(3):320. doi:10.1007/s00595-019-01947-x
- Moore W. Splanchnic and Renal Artery Aneurysms. In: Vascular and Endovascular Surgery: A Comprehensive Review. Philadelphia, PA: Elsevier Saunders; 2013:695-707.
- Belli AM, Markose G, Morgan R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Intervent Radiol. 2012;35(2):234-243. doi:10.1007/s00270-011-0201-3
- Aburahma AF, Campbell JE, Stone PA, et al. Perioperative and late clinical outcomes of percutaneous transluminal stentings of the celiac and superior mesenteric arteries over the past decade. J Vasc Surg. 2013;57(4):1052-1061. doi:10.1016/j.jvs.2012.10.082
- Foley TR, Rogers RK. Endovascular Therapy for Chronic Mesenteric Ischemia. Curr Treat Options Cardiovasc Med. 2016;18(6):39. doi:10.1007/s11936-016-0463-9
- Mitchell EL, Chang EY, Landry GJ, Liem TK, Keller FS, Moneta GL. Duplex criteria for native superior mesenteric artery stenosis overestimate stenosis in stented superior mesenteric arteries. J Vasc Surg. 2009;50(2):335-340. doi:10.1016/j.jvs.2008.12.071
- Aburahma AF, Campbell JE, Stone PA, et al. Perioperative and late clinical outcomes of percutaneous transluminal stentings of the celiac and superior mesenteric arteries over the past decade. J Vasc Surg. 2013;57(4):1052-1061. doi:10.1016/j.jvs.2012.10.082
- Zelenock GB, Stanley JC. Splanchnic artery aneurysms. In: Rutherford RB, ed. Vascular Surgery. Phildalphia, PA: Elsevier; 2000:1369-1382.
- Kim SK, Lee J, Duncan JR, Picus DD, Darcy MD, Sauk S. Endovascular treatment of superior mesenteric artery pseudoaneurysms using covered stents in six patients. AJR Am J Roentgenol. 2014;203(2):432-438. doi:10.2214/AJR.13.11644
- Chaer RA, Abularrage CJ, Coleman DM, et al. The Society for Vascular Surgery clinical practice guidelines on the management of visceral aneurysms. J Vasc Surg. 2020;72(1S):3S-39S. doi:10.1016/j.jvs.2020.01.039
Authors
Frey A; Heidepriem R; McCord RS
Author Affiliation
Department of Surgery, Brookwood Baptist Health System, Birmingham, AL 35211
Corresponding Author
Andrew Frey, DO
Department of Medical Education
Brookwood Baptist Health
833 Princeton Avenue, SW POB III
Birmingham, AL 35211
Phone: (205) 427-2141
Email: andrew.frey@bhsala.com
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: August 17, 2020
Revision received: October 15, 2020
Accepted: November 1, 2020