Discussion
Internal hernias commonly cause small bowel obstruction after abdominal operations, especially after operations reconfiguring the gastrointestinal tract, such as the laparoscopic Roux-en-Y gastric bypass (LRYGB).6 Data concerning internal hernias from duodenojejunostomies is scarce; therefore, much of the knowledge regarding internal hernias is derived from bariatric complications. In laparoscopic bariatric procedures, internal hernias have been found to occur in up to 5% of patients.7 Stenberg et al. showed in a randomized controlled trial that the closure of surgically created mesenteric defects reduced the incidence of internal hernias at the three-year postop mark. The cumulative incidence of reoperation for internal hernia complications was significantly reduced in the closure arm compared to the non-closure group. Due to this significant result, the authors recommended routine closure of all mesenteric defects created or discovered during laparoscopic gastric bypass surgery. However, it is important to note that in the same study, they also found that closure of the mesenteric defects increased kinking of the jejunojejunostomy, which increased the incidence of early small bowel obstruction.1
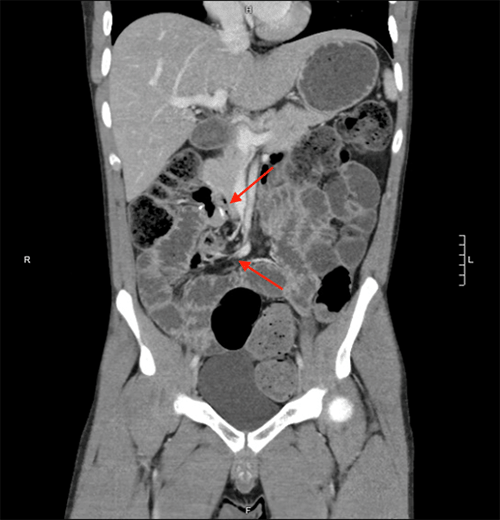
In our patient, we found a mesenteric defect from his laparoscopic duodenojejunostomy that had not been closed, allowing the internal hernia to form. This defect was identified on CT by the presence of the mesenteric swirl sign, which according to the literature, is the most sensitive (78-100%) and specific (80-90%) for diagnosing internal hernias when compared to other radiographic signs. Other radiographic signs, such as the hurricane eye sign, mushroom sign, signs of small bowel obstruction, clustered small bowel loops, or enlarged mesenteric lymph nodes, had good specificities (70-100%) but had overall low sensitivities (0-44%).8,9
Al Harakeh et al. found that there were also differences in bowel obstruction and internal hernia formation rates depending on whether patients received an LRYGB routing the Roux limb via a retrocolic/retrogastric (RC/RG) versus an antecolic/antegastric (AC/AG) position. Those in the RC/RG group had increased rates of bowel obstruction and internal hernias when compared to the AC/AG group. This finding further supports the idea that surgical techniques and decisions made to close or not to close defects impact patient outcomes.
Conclusion
This case study demonstrates an unusual circumstance of internal hernia that provides support for the closure of defects in the mesentery found or created during any abdominal operation, whether bypass surgeries or duodenojejunostomies, to prevent reoperation due to small bowel obstruction. Closing the mesentery defect at the time of this patient's duodenojejunostomy could have possibly prevented the subsequent internal hernia and emergency surgery.
Lessons Learned
We believe that this case study further supports the routine closure of mesentery defects during gastrointestinal surgery to reduce the incidence of reoperations, particularly in a case where the patient was at higher risk for internal herniation due to mobilization of a large amount of bowel in previous surgeries.
References
- Stenberg E, Szabo E, Ågren G, et al. Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet. 2016;387(10026):1397-1404. doi:10.1016/S0140-6736(15)01126-5
- de la Cruz-Muñoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R. Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7(2):176-180. doi:10.1016/j.soard.2010.10.003
- Sharma H, Marwah S, Singla P, Garg A, Bhukkal B. Roux-en-Y duodenojejunostomy for surgical management of isolated duodenal obstruction due to chronic pancreatitis. Int J Surg Case Rep. 2017;31:209-213. doi:10.1016/j.ijscr.2017.01.008
- Chittawadagi B, Senthilnathan P, Jankar SV, Sabnis SC, Parthasarathi R, Palanivelu C. Laparoscopic Roux-en Y duodenojejunostomy: A safe and physiological treatment for symptomatic annular pancreas in adults [published online ahead of print, 2019 Jan 4]. J Minim Access Surg. 2019;16(2):121-125. doi:10.4103/jmas.JMAS_245_18
- Sato N, Yabuki K, Kohi S, et al. Stapled gastro/duodenojejunostomy shortens reconstruction time during pylorus-preserving pancreaticoduodenectomy. World J Gastroenterol. 2013;19(48):9399-9404. doi:10.3748/wjg.v19.i48.9399
- Nimeri AA, Maasher A, Al Shaban T, Salim E, Gamaleldin MM. Internal Hernia Following Laparoscopic Roux-en-Y Gastric Bypass: Prevention and Tips for Intra-operative Management. Obes Surg. 2016;26(9):2255-2256. doi:10.1007/s11695-016-2267-0
- Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234(3):279-291. doi:10.1097/00000658-200109000-00002
- Iannuccilli JD, Grand D, Murphy BL, Evangelista P, Roye GD, Mayo-Smith W. Sensitivity and specificity of eight CT signs in the preoperative diagnosis of internal mesenteric hernia following Roux-en-Y gastric bypass surgery. Clin Radiol. 2009;64(4):373-380. doi:10.1016/j.crad.2008.10.008
- Lockhart ME, Tessler FN, Canon CL, et al. Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls. AJR Am J Roentgenol. 2007;188(3):745-750. doi:10.2214/AJR.06.0541
- Al Harakeh AB, Kallies KJ, Borgert AJ, Kothari SN. Bowel obstruction rates in antecolic/antegastric versus retrocolic/retrogastric Roux limb gastric bypass: a meta-analysis. Surg Obes Relat Dis. 2016;12(1):194-198. doi:10.1016/j.soard.2015.02.004
- Xu Z, Guo W. [Clinical research progress of mesenteric internal hernia after Roux-en-Y reconstruction]. Zhonghua Wei Chang Wai Ke Za Zhi. 2017;20(3):352-356.
Authors
Hayssen HA; Gao G; Pearl JP
Author Affiliation
University of Maryland Medical Center, Baltimore, MD 21201
Correspondence Author
Hilary Hayssen, MD
Department of Surgery
University of Maryland Medical Center
22. S. Greene Street
Baltimore, MD 21201
Phone: 952-240-1776
Email: hhayssen@som.umaryland.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: June 18, 2020
Revision received: November 8, 2020
Accepted: December 9, 2020