Abstract
Background
A 33-year-old male patient with chronic abdominal pain presented for surgical consultation.
Summary
Our patient presented for evaluation of abdominal pain. He complained of dull right upper quadrant pain with episodes of cramping and burning that would intermittently radiate to his back. These flares would last around two hours, occur one to two times a week, and were precipitated by fat-containing foods. His symptoms became increasingly severe over the past two years. At the time of presentation, he had undergone an extensive workup of his symptoms, including unremarkable lab work, normal esophagogastroduodenoscopy, colonoscopy, capsule endoscopy, abdominal MRI, ultrasound, and CT imaging. A hepatobiliary iminodiacetic acid scan with cholecystokinin was reported as normal, with a calculated gallbladder ejection fraction of 99%. Given clinical history consistent with biliary colic and a workup notable for elevated gallbladder ejection fraction, we proceeded with laparoscopic cholecystectomy as the definitive treatment for the patient's biliary hyperkinesia. The procedure was completed without complication. Postoperatively, the patient reported a complete resolution of his symptoms. The final pathology findings were significant for chronic cholecystitis. While the etiology of biliary hyperkinesia and its association with chronic cholecystitis remains poorly documented, our case demonstrates a patient with elevated gallbladder ejection fraction that benefited from cholecystectomy.
Conclusion
This patient presented with clinical findings consistent with biliary disease with unremarkable workup other than HIDA-CCK with a gallbladder ejection fraction of 99%. Cholecystectomy resolved the patient's symptoms and is a valid consideration in patients with biliary colic with biliary hyperkinesia. Elevated GBEF can be associated with chronic cholecystitis.
Key Words
biliary hyperkinesia; cholecystectomy; chronic cholecystitis
Case Description
Patients presenting with symptoms consistent with biliary colic typically describe cramping right upper quadrant pain with possible radiation to the back. Food may trigger episodes and last from 30 minutes to six hours.1-3 Standard workup includes right upper quadrant ultrasound, and those with positive findings such as gallstones are typically treated with cholecystectomy.1 Patients with a negative ultrasound require further evaluation, which may include a hepatobiliary iminodiacetic acid scan with cholecystokinin (HIDA-CCK) to calculate gallbladder ejection fraction (GBEF). Biliary dyskinesia is diagnosed when GBEF < 35-40% and is an accepted indication for surgical intervention.1-9 However, recent studies suggest that patients with elevated GBEF, or biliary hyperkinesia, also benefit from cholecystectomy.3-9 While the exact etiology of biliary hyperkinesia is unknown, a pathological evaluation can demonstrate chronic cholecystitis.4-9
The patient is a 33-year-old White male with a two-year history of dull epigastric pain with episodes of severe cramping right upper quadrant (RUQ) pain intermittently radiating to his back. These flares occurred one to two times a week, lasted from two to several hours, and were often precipitated by meals. He also endorsed nausea with occasional vomiting. Antacids provided minimal relief.
The patient entered our health system seeking a second opinion for his abdominal symptoms. At the time of presentation, he had already undergone an extensive outpatient workup with gastroenterology at another institution. His outside HIDA-CCK was reportedly normal. Esophagogastroduodenoscopy with gastric biopsy was negative. A colonoscopy showed an ulcer in the terminal ileum, possibly consistent with Crohn's etiology; however, this was not supported by pathology, which demonstrated mild focal ileitis. He then underwent a capsule endoscopy, which was reported as normal without any ulcers, strictures, masses, or blood seen. RUQ ultrasound and CT abdomen/pelvis were unremarkable. He was also evaluated for food allergies and even moved out of his house to eliminate environmental factors. Family history was significant for a grandfather that had undergone cholecystectomy.
Upon referral, our GI team repeated blood work, including CBC, CMP, lipase, IBD serology, and inflammatory markers that were normal. A repeat RUQ ultrasound was unremarkable. MRI enterography showed no evidence of acute bowel inflammation, obstruction, or penetrating disease. HIDA-CCK was repeated and reported as normal with GBEF 99% with mild reproduction of his symptoms during the exam. At this time, the patient was referred for surgical evaluation.
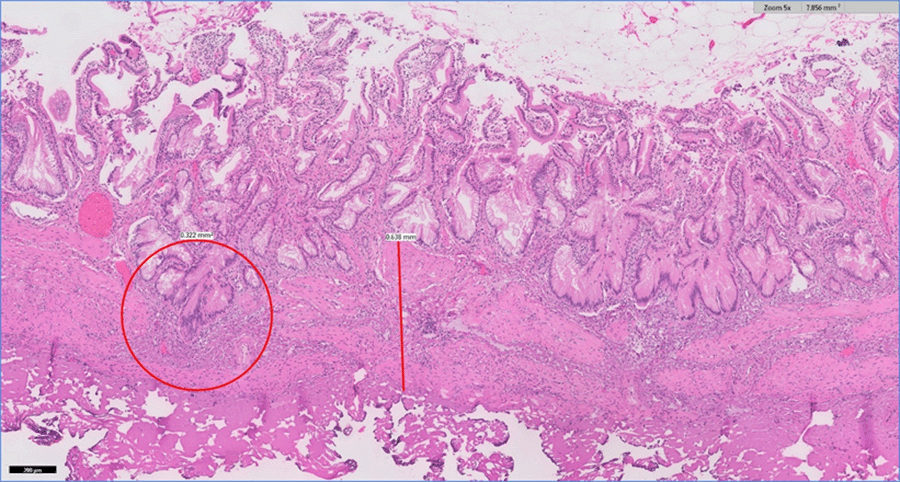
The patient's physical exam was unremarkable. He appeared well-developed, with no acute distress. He did not have scleral icterus. His abdomen was soft, nondistended, nontender, with a negative Murphy's, and no masses, hernia, or scars. BMI 35.14 kg/m2. After carefully discussing the risks and benefits of surgical intervention, the patient underwent laparoscopic cholecystectomy. The procedure was performed without complication, and no abnormalities of the gallbladder or surrounding structures were encountered intraoperatively. The patient was evaluated postoperatively at two-week follow-up and reported a complete resolution of his symptoms. He noted continued pain relief and improved food tolerance at four-week and five-month assessments. His surgical pathology was significant for chronic cholecystitis, as illustrated in Figure 1.
Figure 1. Pathologic Findings of Chronic Cholecystitis at 5x Magnification. Published With Permission
Discussion
Biliary pain is a common indication for surgical referral.1-3 Patients with symptoms of gallbladder disease classically present with intermittent right upper quadrant pain with possible radiation to the back that meals may precipitate.1-4 Patients with symptoms of biliary colic undergo initial evaluation with ultrasound to rule out gallstones and structural pathology. A negative ultrasound necessitates further workup, often with HIDA-CCK, to evaluate for functional gallbladder disorders (FGBD).1-9 A decreased gallbladder ejection fraction, typically defined as less than 35-40%, supports the diagnosis of biliary dyskinesia.1-3 Cholecystectomy remains the definitive treatment for biliary dyskinesia since first described in 1991.1-3,5
Though first noted in 1999, there are limited reports documenting cholecystectomy as the management of biliary hyperkinesia (GBEF > 80%).4-9 In recent studies, patients presenting with biliary colic and negative ultrasound with elevated GBEF on HIDA-CCK report resolution or improvement of their symptoms following cholecystectomy.4-9 Contrary to patients with decreased GBEF, patients with symptomatic biliary hyperkinesia may not receive a surgical referral, and patients that undergo medical management report continued pain.5 Our patient reported mild reproduction of his symptoms with HIDA-CCK, which remains of undetermined significance in predicting benefit from surgery and chronic cholecystitis pathology.4-5,7
While the pathophysiology of biliary hyperkinesia is poorly understood, one proposed etiology is that patients with greater CCK production or density/activity of CCK receptors trigger intense contraction of the gallbladder, causing elevated intraluminal pressure, pain, and inflammation with stimulation.5-6,9 As observed in our patient, many studies have documented chronic cholecystitis on surgical pathology.3-9 Thickening of the tunica muscularis may additionally be noted.5 A summary of results from the current literature is presented in Table 1.
Conclusion
Cholecystectomy is an appropriate consideration for patients with acalculous biliary colic and evidence of biliary hyperkinesia.
Lessons Learned
Patients with biliary pain, negative ultrasound, and HIDA-CCK > 80% benefit from cholecystectomy. Biliary hyperkinesia appears to be associated with chronic cholecystitis.
Authors
Black C; Fann SA
Author Affiliations
Department of Surgery, Medical University of South Carolina, Charleston, SC 29407
Corresponding Author
Collin Black, PA-C, MPAS
Department of Surgery
Clinical Science Building, Ste. 420
96 Jonathan Lucas Street
Charleston, SC 29407
Email: blackc@musc.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: September 28, 2020
Revision received: December 1, 2020
Accepted: January 19, 2021
References
- Cafasso DE, Smith RR. Symptomatic cholelithiasis and functional disorders of the biliary tract. Surg Clin North Am. 2014;94(2):233-256. doi:10.1016/j.suc.2013.12.001
- Cotton PB, Elta GH, Carter CR, Pasricha PJ, Corazziari ES. Rome IV. Gallbladder and Sphincter of Oddi Disorders [published online ahead of print, 2016 Feb 19]. Gastroenterology. 2016;S0016-5085(16)00224-9. doi:10.1053/j.gastro.2016.02.033
- Clark CJ. An Update on Biliary Dyskinesia. Surg Clin North Am. 2019;99(2):203-214. doi:10.1016/j.suc.2018.11.004
- Bates JA, Dinnan K, Sharp V. Biliary hyperkinesia, a new diagnosis or misunderstood pathophysiology of dyskinesia: A case report. Int J Surg Case Rep
- Pillenahalli Maheshwarappa R, Menda Y, Graham MM, Boukhar SA, Zamba GKD, Samuel I. Association of gallbladder hyperkinesia with acalculous chronic cholecystitis: A case-control study. Surgery. 2020;168(5):800-808. doi:10.1016/j.surg.2020.06.005
- Saurabh S, Green B. Is hyperkinetic gallbladder an indication for cholecystectomy?. Surg Endosc. 2019;33(5):1613-1617. doi:10.1007/s00464-018-6435-2
- Lindholm EB, Alberty JB, Hansbourgh F, Upp JR, Lopoo J. Hyperkinetic gallbladder: an indication for cholecystectomy?. Am Surg. 2013;79(9):882-884.
- Gazzetta J, Fan B, Bonner P, Galante J. Cholecystectomy for Biliary Hyperkinesia. Am Surg. 2019;85(2):219-222.
- Nasri B, Glass T, Singh K, Saxe J. Biliary hyperkinesia: an indication for cholecystectomy?. Surg Endosc. 2021;35(7):3244-3248. doi:10.1007/s00464-020-07757-4