Abstract
Background
Left paraduodenal hernias (L-PDHs) occur through the fossa of Landzert, a rare congenital mesenteric defect caused by the non-fusion of the mesocolon and mesentery of the fourth part of the duodenum to the posterior parietal peritoneum. Intestinal obstruction caused by L-PDHs is associated with a high risk of intestinal strangulation and significant mortality. After reducing the hernia contents, closure of the hernia defect is important for preventing recurrence. We describe a novel technique in which a pedicled omental flap is used as an alternative technique to close the hernia defect.
Summary
A 70-year-old man with no prior abdominal surgeries was taken emergently to the operating room after presenting with an acute abdomen and computer tomography findings suggestive of an L-PDH. At surgery, several loops of upper jejunum were found to be herniated and incarcerated through the para-duodenal fossa of Landzert. After the hernia sac was quickly opened, the incarcerated but viable small bowel loops were retrieved from the hernia defect. Attempts at closure with sutures of the large L-PDH defect by re-approximation of the mesenteric defect to the retroperitoneum were unsuccessful as sutures did not hold due to increased tension. Faced with the inability of suture closure of the hernia defect, a novel approach was performed by placing an omental flap over the L-PDH defect, which was secured in place with interrupted absorbable sutures. Subsequently, the patient has had an uneventful recovery without the recurrence of his hernia.
Conclusion
Maintaining a clear understanding of the embryology and anatomy of L-PDHs is important for the successful repair and avoidance of intraoperative injuries. The omental flap could be used as a dependable and durable technique for the repair of L-PDHs.
Key Words
acute abdomen; internal hernia; incarcerated hernia
Case Description
Left paraduodenal hernias (L-PDHs) are rare congenital internal abdominal hernias resulting from failure of fusion of the inferior mesentery to the parietal peritoneum and an associated abnormal embryonic rotation of the midgut1 that leads to herniation of the small bowel between the mesocolon and the retroperitoneum. Intestinal obstruction caused by L-PDHs is associated with a high risk of intestinal strangulation2,3 and an overall mortality of 20% to 50%.4,5 The surgical management of L-PDHs consists of timely reduction of the hernia contents followed by management of the hernia defect.
A 70-year-old man with no prior abdominal surgeries presented to our emergency department with several hours of sudden onset severe pain in the left upper quadrant of the abdomen and obstipation without nausea or vomiting. On physical examination of the abdomen, the patient had severe tenderness in the left upper quadrant, with involuntary guarding across the entire abdomen, without rebound tenderness.
On presentation, he was afebrile, with a normal heart rate (60 beats/min) and hypertensive (156/75 mm Hg). His lactic acid level was 1.97 mmol/L (normal range 0.5 to 1.8), and the white blood cell count was 11.5 K/mm3 (normal range 4.5 to 10.0) without a neutrophil left shift. The remainder of the blood counts and chemistry were normal.
A noncontrast computed tomography (CT) scan of the abdomen obtained in the emergency department showed distended small bowel loops in the left upper quadrant that appeared clustered in the left pararenal space with mild crowding, congestion, and stretching of the mesentery suggestive of an internal hernia causing an acute intestinal obstruction (Figure 1). Given the presence of an acute abdomen, the patient was taken emergently to the operating room for abdominal exploration.
Figure 1. Coronal CT Scan of Abdomen. Published with Permission
At surgery, several loops of upper jejunum were found to be herniated and incarcerated into the para-duodenal fossa of Landzert—a defect between the ligament of Treitz, the fourth portion of the duodenum, and the mesentery of the transverse and descending colon (Figure 2). After the hernia sac was quickly opened, we retrieved the incarcerated small bowel loops from the hernia defect – they were noted to be bruised and congested but intact and well-perfused.
Figure 2. Fossa of Landzert with Inferior Mesenteric Vein and Ascending Left Colic Artery Running Along Lateral Free Edge. Published with Permission
While evaluating our options for closure of this large (10 × 15cm) L-PDH defect, we determined that the size and topography of the defect would result in significant tension if we attempted to perform a suture repair by re-approximating the mesenteric defect to the retroperitoneum. Indeed, attempts at simple closure with sutures were unsuccessful as sutures did not hold.
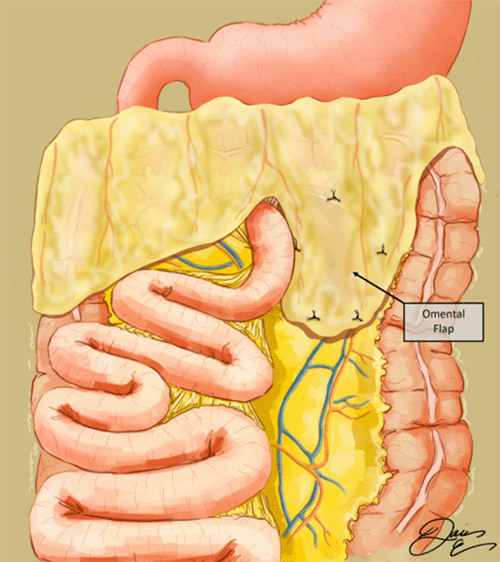
Faced with the inability to perform a tension-free suture repair of the hernia defect, a novel approach was performed using an omental flap to cover the hernia defect. The omentum was divided along avascular planes to create a 15 × 20 cm flap that was placed over the L-PDH defect and secured with interrupted absorbable sutures (Figure 3). Subsequently, the patient had an uneventful recovery: he was discharged home on postoperative day 4 and had no complications during postoperative follow-up visits.
Figure 3. Omental Flap Secured Over Left Paraduodenal Hernia Defect. Published with Permission
Discussion
Paraduodenal hernias account for 53% of all internal abdominal hernias and are most often diagnosed in males during their fourth to sixth decades of life.6 Approximately 75% of these hernias occur to the left of the ligament of Treitz (6) through the fossa of Landzert. This potential space is a rare congenital mesenteric defect caused by the non-fusion of the mesocolon and mesentery of the fourth part of the duodenum to the posterior parietal peritoneum. It is present in about 2% of the population7 and is found to the left of the duodenojejunal junction at the confluence of the descending mesocolon, transverse mesocolon, and small bowel mesentery.8,10 The inferior mesenteric vein (IMV) and the ascending left colic artery run along the lateral free edge of the fossa (Figure 2). An L-PDH occurs when the viscera protrude posteriorly into this space.
The clinical features of L-PDHs are nonspecific and vary depending on the degree of small bowel entrapment. Most patients are asymptomatic; the hernia is discovered incidentally in imaging studies, intraoperatively, or during autopsy.9 Some patients experience chronic intermittent post-prandial pain or indigestion, often dating back to childhood,10 likely due to intermittent herniation. The rare prevalence of the L-PDHs, their non-specific presenting symptoms, and the lack of physician awareness of congenital internal hernias make the clinical diagnosis challenging and lead to diagnostic delays. Thus, the average time to diagnose L-PDHs is 21 to 23 months.5,11
Undiagnosed and untreated L-PDHs have a 50% lifetime risk of acute small bowel obstruction,5 with a high risk of strangulation,2,3 a 20% risk of bowel necrosis,12,13 and high mortality.4,5 Therefore, it is crucial to maintain a high index of suspicion for L-PDHs, especially when partial or complete intestinal obstruction occurs in patients without previous abdominal surgeries.3
Given the challenges of clinical diagnosis of L-PDHs, diagnosis is based on pathognomonic features on CT scanning. The characteristic CT findings include an abnormal cluster or sac-like mass of dilated small bowel loops to the left of the ligament of Treitz and crowded, engorged, and stretched mesenteric vessels supplying the herniated small bowel segments.14,15
The surgical treatment of L-PDHs includes reduction of the herniated small bowel loops, resection of any necrotic bowel, and management of the hernia orifice. When the hernia opening is very narrow, incising the avascular inferior border of the hernia or even division of the inferior mesenteric vein running along the left edge of the defect can be used to facilitate a prompt reduction of the hernia contents.16-18
Described techniques for the management of the hernia orifice after reduction of the hernia contents consist of obliteration, enlargement, or closure of the defect. Large hernia defects can be obliterated by reflecting and transfixing the hernia sac to the adjacent retroperitoneum so that the emptied hernia cavity becomes part of the peritoneal cavity.19 This effectively obliterates the hernia orifice to prevent hernia recurrence.
Enlargement of narrow defects is performed by dividing the inferior border of the hernia, followed by obliteration of the hernia sac by suture apposition to the retroperitoneum.20 However, this approach risks damaging the IMV and branches of the left colic artery.4
The most commonly reported approach to managing L-PDH defects is closure with sutures (non-absorbable > absorbable) either in a continuous or interrupted fashion.16,21-26 Because the IMV is very close to the lateral free edge of the hernia orifice, sutures are placed adjacent or through the sheath of the IMV,27 thus increasing the risk of venous injury.16 Furthermore, when the topography of the hernia defect is unsuitable for tension-free suture closure, suturing can increase the risk of hernia recurrence. In one reported case, an L-PDH recurred after a suture closure and required tension-free repair with Gore-Tex mesh.16
Herein, we report the successful use of an omental flap as a novel alternative technique for repairing L-PDH defects. The use of an omental flap in this situation has several potential advantages. First, because the omental flap overlaps the hernia defect, it can be secured in place with sutures away from the vascular structures running along the edges of the hernia defect, thus minimizing the risk of vascular injuries. Second, an omental flap would allow a tension-free repair of the hernia defects when closure with sutures under no undue tension is not feasible. Third, the omental flap could be used as an alternative to mesh because it avoids the risk of infection and the costs associated with mesh use. Fourth, using an omental flap could decrease the need to enlarge the L-PDH defect and its inherent risk of vascular injury.
To our knowledge, our case represents the first report describing the omental flap utilization for repairing L-PDHs. This case report is significant because it presents a quick, safe, and durable option for managing L-PDHs. The omental flap is a useful addition to the armamentarium of techniques for surgeons who need to repair L-PDHs with anatomical features that prevent the use of other repair techniques.
Conclusion
L-PDHs are rare and present a diagnostic challenge. A high index of clinical suspicion and preoperative CT imaging is essential for their timely diagnosis and surgical treatment. Maintaining a clear understanding of the embryology and anatomy of these hernias is important for the successful repair and avoidance of intraoperative injuries. The omental flap could be used as a dependable and durable technique for the repair of L-PDHs.
Lessons Learned
L-PDHs represent a significant surgical challenge. Surgeons should be prepared to employ all possible approaches to repair hernia defect, including the omental flap successfully used in our case.
Authors
Lin Ba,b, Eble DJc; Riley MSa,d; He Ka,d; Kristo Ga,d
Author Affiliations
- Department of Surgery, Veterans Affairs Boston Healthcare System, Boston, MA 02132
- Department of Surgery, Boston Medical Center, Boston University Medical School, Boston, MA 02118
- Department of Surgery, University of Washington, Seattle, WA 98195
- Department of Surgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02115
Corresponding Author
Gentian Kristo, MD, MPH, FACS
Department of Surgery
Veterans Affairs Boston Healthcare System (112-C)
1400 VFW Parkway
West Roxbury, MA 02132
Email: gentian.kristo@va.gov
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Acknowledgments
Dr. Danielle J. Eble (University of Washington) prepared the drawn illustrations for the report.
Received: February 15, 2021
Accepted for publication: May 5, 2021
References
- Ghahremani GG. Internal abdominal hernias. Surg Clin North Am. 1984;64(2):393-406. doi:10.1016/s0039-6109(16)43293-7
- Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152(3):279-285. doi:10.1016/0002-9610(86)90258-8
- Fan HP, Yang AD, Chang YJ, Juan CW, Wu HP. Clinical spectrum of internal hernia: a surgical emergency. Surg Today. 2008;38(10):899-904. doi:10.1007/s00595-007-3756-5
- Khan MA, Lo AY, Vande Maele DM. Paraduodenal hernia. Am Surg. 1998;64(12):1218-1222.
- Tong RS, Sengupta S, Tjandra JJ. Left paraduodenal hernia: case report and review of the literature. ANZ J Surg. 2002;72(1):69-71. doi:10.1046/j.1445-2197.2002.02300.x
- Ghahremani GG. Abdominal and pelvic hernias. In: Gore RM, Levine MS, eds. Textbook of gastrointestinal radiology, 2nd ed. Philadelphia, PA: Saunders. 2000:1993–2009.
- Downes R, Cawich SO. A case of a paraduodenal hernia. Int J Surg Case Rep. 2010;1(2):19-21. doi:10.1016/j.ijscr.2010.06.003
- Okino Y, Kiyosue H, Mori H, et al. Root of the small-bowel mesentery: correlative anatomy and CT features of pathologic conditions. Radiographics. 2001;21(6):1475-1490. doi:10.1148/radiographics.21.6.g01nv121475
- Manji R, Warnock GL. Left paraduodenal hernia: an unusual cause of small-bowel obstruction. Can J Surg. 2001;44(6):455-457.
- Meyers MA. Dynamic radiology of the abdomen: normal and pathologic anatomy, 4th ed. New York, NY: Springer-Verlag, 1994.
- Brigham RA, Fallon WF, Saunders JR, Harmon JW, d'Avis JC. Paraduodenal hernia: diagnosis and surgical management. Surgery. 1984;96(3):498-502.
- Hirasaki S, Koide N, Shima Y, et al. Unusual variant of left paraduodenal hernia herniated into the mesocolic fossa leading to jejunal strangulation. J Gastroenterol. 1998;33(5):734-738. doi:10.1007/s005350050164
- Nishida T, Mizushima T, Kitagawa T, Ito T, Sugiura T, Matsuda H. Unusual type of left paraduodenal hernia caused by a separated peritoneal membrane. J Gastroenterol. 2002;37(9):742-744. doi:10.1007/s005350200121
- Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186(3):703-717. doi:10.2214/AJR.05.0644
- Takeyama N, Gokan T, Ohgiya Y, et al. CT of internal hernias. Radiographics. 2005;25(4):997-1015. doi:10.1148/rg.254045035
- Palanivelu C, Rangarajan M, Jategaonkar PA, Anand NV, Senthilkumar K. Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008;12(6):649-653. doi:10.1007/s10029-008-0376-y
- Erdas E, Pitzalis A, Scano D, Licheri S, Pomata M, Farina G. Diagnosis and treatment of symptomatic right paraduodenal hernia: report of a case. Surg Today. 2014;44(1):192-196. doi:10.1007/s00595-012-0483-3
- Blachar A, Federle MP, Dodson SF. Internal hernia: clinical and imaging findings in 17 patients with emphasis on CT criteria. Radiology. 2001;218(1):68-74. doi:10.1148/radiology.218.1.r01ja5368
- Cundy TP, Di Marco AN, Hamady M, Darzi A. Giant left paraduodenal hernia. BMJ Case Rep. 2014;2014:bcr2013202465. Published 2014 May 2. doi:10.1136/bcr-2013-202465
- Downes R, Cawich SO. A case of a paraduodenal hernia. Int J Surg Case Rep. 2010;1(2):19-21. doi:10.1016/j.ijscr.2010.06.003
- Zonca P, Maly T, Mole DJ, Stigler J. Treitz's hernia. Hernia. 2008;12(5):531-534. doi:10.1007/s10029-008-0339-3
- Siddika A, Coleman AH, Pearson TE. Laparoscopic repair of left paraduodenal hernia. J Surg Case Rep. 2013;2013(10):rjt079. Published 2013 Oct 4. doi:10.1093/jscr/rjt079
- Sleiman Y, El-Kheir A, El-Khoury M, Hamdach O, Ismail L, Allouch M. Small bowel obstruction secondary to left paraduodenal hernia: A case report and literature review. Int J Surg Case Rep. 2018;53:29-31. doi:10.1016/j.ijscr.2018.10.018
- Martins A, Gonçalves Á, Almeida T, Gomes R, Lomba J, Midões A. Left Paraduodenal Hernia. J Gastrointest Surg. 2018;22(5):925-927. doi:10.1007/s11605-017-3626-4
- Shadhu K, Ramlagun D, Ping X. Para-duodenal hernia: a report of five cases and review of literature. BMC Surg. 2018;18(1):32. Published 2018 May 30. doi:10.1186/s12893-018-0365-8
- Cho YM, Aksakal G, Ashour MAT, Moore S. Closed loop bowel obstruction secondary to left paraduodenal hernia (of Landzert). BMJ Case Rep. 2019;12(12):e232134. Published 2019 Dec 5. doi:10.1136/bcr-2019-232134
- Sakamoto T, Lefor AK. Laparoscopic reduction and repair of a left paraduodenal hernia. BMJ Case Rep. 2019;12(12):e232098. Published 2019 Dec 15. doi:10.1136/bcr-2019-232098