Editor’s note: The 14 ACS Advisory Councils, which serve as liaisons in the communication of information to and from surgical societies and the Regents, periodically submit articles on the notable initiatives taking place in their respective specialties. This feature is a submission from the Advisory Council for Gynecology and Obstetrics.
Ovarian cancer is one of the deadliest cancers in the US, with 19,710 cases and 13,270 anticipated deaths in 2023. It ranks as the fifth-leading cause of cancer death in women due primarily to the advanced stage at diagnosis.
Despite extensive research and efforts, there is still not an effective ovarian cancer screening test. In fact, the United States Preventive Services Task Force, US Food and Drug Administration, and organizations focused on ovarian cancer, such as the American College of Obstetricians and Gynecologists (ACOG) and Society of Gynecologic Oncology (SGO), have strongly recommended against ovarian cancer screening because it has not been proven effective in improving outcomes and may be harmful to women.
Most recently, the Ovarian Cancer Research Alliance released an Ovarian Cancer Screening and Symptom Awareness Consensus Statement, which provides an overview of current data and recommendations.
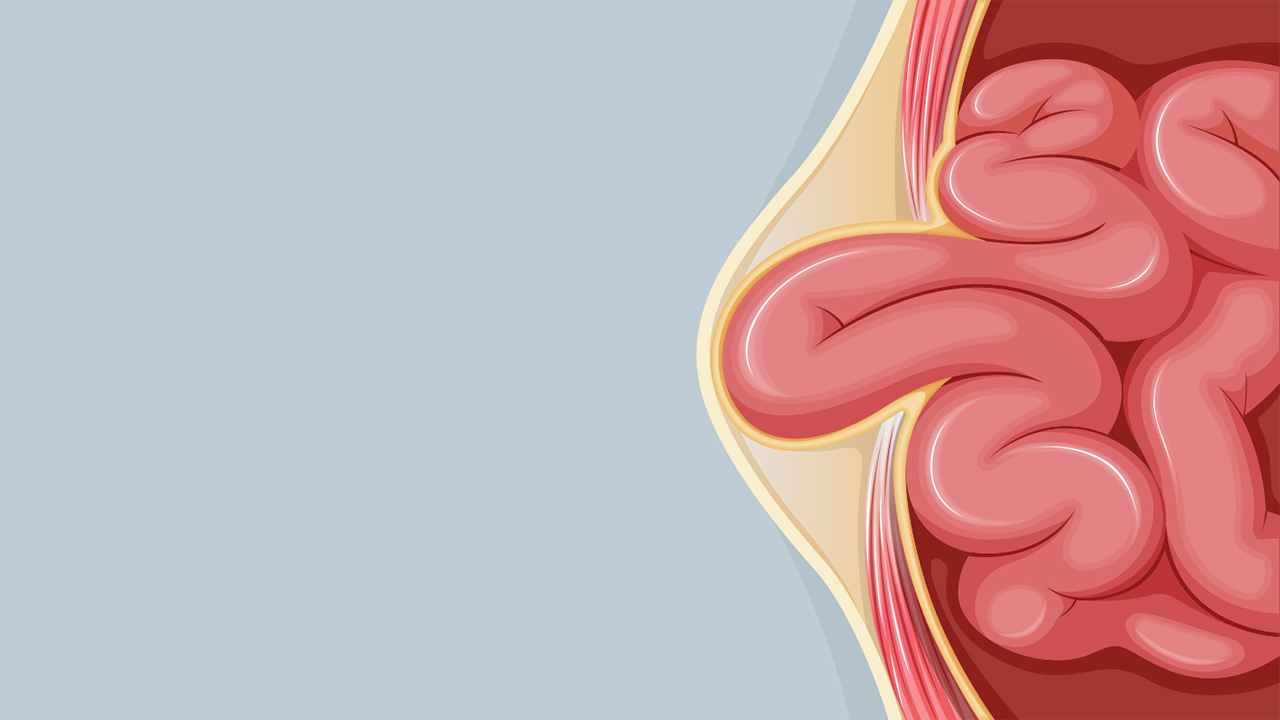
It has become apparent that while ovarian, fallopian tube, and primary peritoneal cancers are often lumped together, about 65% of the most common form of high-grade serous “ovarian” cancer appear to originate from the fallopian tube, where it progresses from precancerous lesions (serous tubal intraepithelial carcinoma, so-called STIC lesions) to cancer. These microscopic cells from the tubes then disseminate into the peritoneal cavity and implant as metastatic lesions on the ovaries, omentum, and other structures, which explains the 70%-80% rate of late stage at diagnosis.
On a positive note, despite lack of effective screening, ovarian cancer incidence rates decreased 1%-2% per year from 1990 to 2010 and decreased even further at 3% per year from 2015 to 2019. The notable decline in ovarian cancer incidence and mortality likely stems from the following phenomena:
- Increased recognition that almost 24% of ovarian cancer stem from inherited cancer predisposition syndromes and identifying affected patients (for example, BRCA mutations)
- Cascade genetic testing of these patients and high-risk families to allow implementation of proven and effective risk reduction measures (both chemoprevention and surgery)
- Positive impact of more widespread use of oral contraceptives, which decrease ovarian cancer by 50% in both normal and high-risk women
- Increased uptake of opportunistic salpingectomies in normal risk women who are undergoing other surgical procedures
SGO and ACOG have strongly promoted opportunistic salpingectomies for patients who have completed childbearing and are undergoing other pelvic surgeries like C-section, ovarian surgery, hysterectomy, or tubal ligation.
Investigators are also starting to look at how more women could undergo this potentially lifesaving procedure and whether it is acceptable and feasible to do at the time of appendectomy, cholecystectomy, or other non-gynecologic abdominal surgeries. Preliminary data suggest that it could be feasible at cholecystectomy (and potentially appendectomy, ventral hernia repair, and bariatric surgery is), it is acceptable to patients, and could result in even further reductions in ovarian cancer incidence.
What can any surgeon do to help decrease ovarian, fallopian, and primary peritoneal cancers?
- Routinely ask all patients about personal and family cancers (particularly, breast, ovarian, pancreatic, uterine, and colon cancers) and refer to genetic counseling/testing to identify high risk patients and their families
- Discuss opportunistic salpingectomy with any patient with fallopian tubes who does not desire future fertility and is undergoing a planned abdominal surgery
Implementing these steps could help reduce the devasting impact of ovarian cancer for women as prevention remains the superior option for better cancer outcomes compared to screening or treatment after diagnosis.
Dr. Susan Modesitt is director of gynecologic oncology division and Leach Hendee Endowed Professor at Emory University in Atlanta, GA.